The structure of the female reproductive system. The structure of the penis in men - what the male organ consists of
In this topic, we will briefly consider the male genitourinary system in general and the structure of the penis (PP) in particular.
Kidneys- the main and most important paired organ of the human urinary system. The kidneys are bean-shaped, measure 10 - 12 x 4 - 5 cm and are located in the retroperitoneal space on the sides of the spine. The right kidney is crossed in half by the line of the right 12th rib, while 1/3 of the left kidney is above the line of the left 12th rib, and 2/3 is below (i.e. the right kidney is located slightly lower than the left). During inhalation and when a person moves from a horizontal to a vertical position, the kidneys shift downwards by 3 - 5 cm. Fixation of the kidneys in a normal position is ensured by the ligamentous apparatus and the supporting effect of the perinephric tissue. The lower pole of the kidneys can be felt with your hands while inhaling in the right and left hypochondrium.
Relative canal The relative canal has the role of an epididymal excretory canal and is an extension of the epididymis. Being part of the sperm cable, it crosses the inguinal canal and enters the pelvic cavity. It connects with the seminal vesicular duct, becoming the ejaculatory duct, which crosses the prostate and opens into the urethra.
Prostate. The prostate is a gland located in the pelvic cavity. Its function is to produce and release substances on the surface of the urethra during the passage of seminal fluid and to act on the seminal fluid itself. Seminal vesicles Seminal vesicles - two, and in abdominal cavity- between the bladder and rectum. They have the function of forming the seminal clot, influencing certain characteristics of the fluid and suppressing any antibody against sperm. Penis The penis and scrotum represent the male external genitalia.
Kidney function:
The main function of the kidneys - excretory - is achieved by the processes of filtration and secretion. In the renal corpuscle from the capillary glomerulus, under high pressure, the contents of the blood along with plasma (except for blood cells and some proteins) are filtered into the Shumlyansky-Bowman capsule. The resulting liquid - primary urine - continues its path through the convoluted tubules of the nephron, in which nutrients (such as glucose, water, electrolytes, etc.) are reabsorbed into the blood, while urea, uric acid and creatine remain in the primary urine. As a result, secondary urine is formed, which goes from the convoluted tubules into the renal pelvis, then into the ureter and bladder. Normally, 1700-2000 liters of blood pass through the kidneys per day, 120-150 liters of primary urine and 1.5-2 liters of secondary urine are formed.
The penis has no bones inside and consists of a fixed root and a free body ending in a more sensitive limb, the throat. At the end it foreskin, where the skin is folded to form a retractable fold. The foreskin is attached to the gland by a flap of skin, which takes its name. The inside of the penis is formed by the urethra, which allows seminal fluid and urine to pass externally and is wrapped in a colander called the corpus spongiosum and two cylinders called the corpora cavernosa, allowing proper blood flow to the penis, ensuring the maintenance of an erection.
Bladder- organ of the human urinary system. The bladder is located in the pelvis behind the pubic bones, above the prostate, and in front of the rectum. Part of the upper and posterior walls of the bladder is covered by the parietal peritoneum.
The right and left ureters approach the posteroinferior surface of the bladder. The neck of the bladder continues into the urethra (urethra).
When full, the bladder may protrude above the pubis. In this condition, the bladder can be felt with your hands in the lower abdomen directly above the pubis in the form of a round formation, when pressed, the urge to urinate occurs. The capacity of the bladder is usually 200 - 400 ml. The inner surface of the bladder is covered with mucous membrane. Between the bladder and the urethra there is a thick circular muscle - the Sphincter; it prevents involuntary urination.
Male urethra - The male urethra extends approximately 20 cm from the bladder to the tip of the penis. It allows the passage of both urine and seminal fluid. Introduction The environment around us is constantly changing its functions in a cyclical and repeatable manner. Just think about constant and cyclical changes environment, which occur within 24 hours with alternation and passage between day and night, or cyclical changes that occur throughout the year, with alternating seasons.
Adaptation to the environment and environmental changes is an important evolutionary mechanism for the survival of every animal species. To better adapt to these environmental changes, plants and animals have developed internal anticipatory rhythms to environmental changes. In mammals, the role of controlling this rhythm has been assigned to a nerve nucleus, the superclastic nucleus of the hypothalamus. This nucleus has electrical discharge activity with a rhythm of about 24 hours. This rhythmicity is transmitted through various efferent routes to all cells in the body, which, as a consequence, change its function.
Bladder function- a reservoir of urine from which it is excreted, that is, it serves to accumulate urine flowing from the kidneys and periodically remove it through the urethra.
Prostate gland (prostate)- This is one of the organs of the male reproductive system. The prostate has the shape of a chestnut, is located in the male pelvis below the bladder, behind the bones of the pubis, in front of the rectum and covers the initial sections of the urethra on four sides. The seminal vesicles are located on the posterior surface of the prostate. The posterior surface of the prostate can be felt with a finger through the anterior wall of the rectum. The prostate, being a gland, produces its own secretion, which enters the lumen of the urethra through the excretory ducts.
This creates a rhythmic synchrony between all biological functions of the body. Obviously, the rhythm of the superclassical core must be synchronous with external environmental conditions, so that the anticipatory internal rhythm coincides with the external state of the environment. In fact, the activity of the superclastic nucleus is synchronized with the surrounding conditions by light information that is perceived by retinal structures that are not representative of vision and reach it through the retino-hypothalamic tract.
Modifications in light exposure resulting from changes in day length are also sensed by the proliferation core to induce a seasonal rhythm in the body's biological functions. If these changes, which optimize energy expenditure and biological function, are ultimately important for the survival of each individual, they are all the more important for the survival of each a separate type animals. The human species, like all other species, follows these rhythms, which are actually little studied and misunderstood, especially in the area of reproduction.
Functions of the prostate:
The main function of the prostate is the production of a special clear, slightly alkaline liquid - prostatic juice, which makes up about 10 - 30% of the volume of sperm. The rest of the semen consists of fluid produced by the seminal vesicles, two sac-like structures located on the sides and back of the prostate. As we have already said, prostatic juice has an alkaline reaction, which is necessary to neutralize the acidic reaction of the vaginal environment.
However, the inherent importance of these rhythms can be evident in the rough observation of our reproductive functions when we consider that a woman's menstrual cycle lasts 28 days, that is, exactly the lunar cycle, and 280 days of pregnancy, that is, the 10 months of the moon. In this article we summarize the evidence that in present moment we have in mind that daily and seasonal rhythms play out at different stages reproductive life, especially in relation to human reproductive life.
Melatonin as a biological transformer of environmental conditions. Research various types showed that a significant part of the environmental influence on the reproduction of various animal species depends on changes in environmental temperature and photoperiod. The mechanisms by which temperature influences reproductive events have not yet been clearly defined, although it has been fairly clear that the mechanism that mediates the effects of photoperiod is mainly due to changes in melatonin secretion at night.
Seminal vesicles:
The left and right seminal vesicles are located on the posterior surface of the prostate on either side of it, behind the bladder, and in front of the rectum. It is possible to palpate with a finger through the anterior wall of the rectum on the sides of the basal sections of the prostate.
They are approached by the vas deferens, which, after joining the seminal vesicles, pass into the ejaculatory ducts, which in turn pass through the prostate and open with their mouths into the lumen of the prostatic urethra on the sides of the seminal tubercle. The tissue of the seminal vesicle has a cellular structure.
Melatonin is produced by the pineal gland in a circadian rhythm. Its secretion is controlled by the hypocalamic nucleus of the hypothalamus and occurs through stimulation of beta-adrenergic receptors located in the pineal gland. The pineal gland releases melatonin in both the cephaloid-rachid fluid and the blood. Cephalide rachid fluid is the primary vehicle through which melatonin reaches the hypothalamus and brain structures, while blood is the primary vehicle through which melatonin reaches all peripheral organs.
Functions of seminal vesicles:
1. Secretion of fructose, the level of which is an indicator of androgen saturation.
Fructose serves as a source of energy to maintain sperm viability and motility.
2. Participation in the mechanism of ejaculation - at the moment of ejaculation, the contents of the seminal vesicles and vas deferens enter the urethra through the ejaculatory ducts, where they are mixed with prostate secretions and excreted.
3. When sexual arousal is not realized, sperm enter the seminal vesicles, where they can be absorbed by spermiophages
Exposure to light, by altering the activity of the superclassical nucleus, rapidly inhibits melatonin secretion. Thus, nighttime melatonin production is reduced in the presence of a long photoperiod, with early morning light inhibiting secretion early and evening light slowing production. In contrast, during seasons with short photoperiods, nighttime melatonin secretion lasts longer. It is these changes in the length of melatonin production that provide a signal that can affect animal and possibly human reproduction.
Bulbourethral (bulbourethral) glands- (Cooper's gland) - a paired organ that secretes a viscous fluid that protects the mucous membrane of the wall of the male urethra from irritation by urine.
The bulbourethral glands are located behind the membranous part of the male urethra, in the thickness of the deep transverse perineal muscle. The glands are spaced from each other at a distance of about 0.6 cm. The bulbourethral gland is round, has a dense consistency and a yellowish-brown color, with a slightly bumpy surface; its diameter is 0.3 - 0.8 cm. These are alveolar-tubular glands. The duct of the bulbourethral gland is thin and long (about 3 - 4 cm).
However, changes in the signal carried by the nocturnal secretion of melatonin do not lead to unambiguous responses in all animals, and different, even opposite effects may occur in different types animals. Thus, the expansion of the signal is sensed as being inhibited by some species of rodents, such as hamsters or mice, and stimulated by other species, such as sheep or monkeys.
Adjustment of reproductive organ development In mammalian species with apparent seasonal reproduction, the development of puberty is highly dependent on photoperiod. For example, in some seasonal rodents puberty begins in the summer when there are many hours of light and short melatonin secretion at night, and is blocked in the winter months when there is a short photoperiod and long melatonin secretion. Although a very long melatonin signal suppresses the development of the sexual pool, maintaining a specific melatonin night signal of a long photoperiod is essential for the development of sexual maturity.
Function of the bulbourethral (bulb) gland:
During sexual arousal, each gland secretes a transparent, viscous mucous secretion (pre-ejaculate), which tastes salty with a sweetish tint. This fluid helps lubricate the urethra for sperm to pass through, it protects the urethral mucosa from urine irritation, neutralizes traces of acidic urine in the urethra, and helps remove any residual urine or foreign matter.
Indeed, in these species, abolishing the short nightmare of melatonin by removing the pineal gland prevents the development of sexual maturity. However, puberty can be induced again in pinesectomized animals by administering melatonin for 4 to 6 hours a day. Various studies show that even in those mammals that do not reproduce closely seasonally, photoperiod and melatonin can influence the developmental process of the lobe. For example, the sexual development of laboratory rats depends on daylight and melatonin production.

Testicles (testes), testicles- These are the male gonads.
The testicles (right and left) are located in the corresponding halves of the scrotum in a man. The spermatic cord, consisting of the testicular membranes, testicular artery, veins of the testicular venous plexus and the vas deferens, approaches the upper pole of each testicle. Along the lateral surfaces of the testicles, from the upper to the lower poles, there are epididymis, which at the lower pole of the testicle continue into the vas deferens. The testicles can be felt with your hands through the skin of the scrotum in the form of round formations of elastic consistency. The epididymis is palpated in the form of ridges on the lateral surface of the testicles.
A short photoperiod with enhanced melatonin signaling counteracts the development of sexual maturity. In contrast, as in rats, sheep and monkeys, the first ovulation occurs in the autumn or winter months with shortening photoperiod and lengthening melatonin. Even in these species, pinectomy interferes with the development of the reproductive organs, which is restored with the introduction of melatonin. There is no information about the influence of seasons on the development of puberty in the human race. This observation was then expanded by further observations indicating an association between destructive pineal tumors and precocious puberty, and conversely, an association between hyperactive pineal cancers and delayed puberty.

The best temperature for testicular function is slightly lower than core body temperature (32°C). Spermatogenesis is less efficient at other, relatively higher or lower temperatures. That is why they are moved outside the abdominal cavity, into the scrotum, which has a number of temperature regulation mechanisms.
Proponents of the inhibitory role of melatonin in the development of puberty emphasize that daily levels of melatonin gradually decrease from childhood to adult life. However, during puberty there is no sudden modification in plasma melatonin levels, and the decrease in circulating levels is explained by the fact that the increase in mass of melatonin mass produced in equal amounts is diluted into a gradually larger volume. On the other hand, studies in patients with early or late puberty have not provided definitive answers.
Testicular function:
The convoluted tubules of the testicles produce male reproductive cells - sperm. The cells are produced from a specialized epithelium, with one cell of this epithelium producing four to eight sperm.
Normally, a sexually mature man of any age produces about 50 thousand sperm per minute. The maturation process of sperm takes approximately 77 days, after which they leave the testicles through thin canals at the top and enter the epididymis, a curving canal with a total length of about 4.5 cm, where they acquire the ability to swim and fertilize the egg. Then the sperm are distilled from the epididymis into the penis through the vas deferens - a tube encased in muscle, about 30 cm long. In some diseases of men, sperm motility is absent or insufficient, which is one of the causes of male infertility.
It is therefore possible that nocturnal increases in melatonin may promote the onset of puberty only when the reproductive axis becomes receptive to its modulatory effects. This possibility is consistent with data observed in primates, where pathological development is delayed by pinallectomy and restored by restoring an appropriate daily melatonin signal. In conclusion, animal data indicate that short photoperiods with long melatonin release stimulate the onset of puberty in sheep and monkeys and conversely inhibit it in rodents.
In addition, the interstitial tissues of the testicle (glandulocytes) produce male sex hormones (androgen) - testosterone. Male sex hormones (androgens) affect sexual behavior (libido and potency).
Vas deferens- is a direct continuation of the epididymal duct, has a length of 45 - 50 cm. Diameter is 3 mm. Consists of mucous, muscular and connective tissue membranes. Thanks to the powerful muscular membrane of the vas deferens, it can be easily felt in the inguinal canal.
Even in species where short photoperiod and prolonged melatonin secretion at night are reproductive inhibitors, the short melatonin signal produced in short nights, for the development of puberty. Daily and seasonal variations in departure and departure routes. Circadian rhythm. Like most biological functions in animals and humans, the beginning of the perimeter shows a daily rhythm with more high frequency at night. In female nonhuman primates, this rhythm reflects the endogenous rhythm of myometrial contractile action, which results from both increased circulating levels of oxytocin and myometrial oxytocin sensitivity.
It is part of the spermatic cord and, together with it, is directed to the external opening of the inguinal canal. After leaving the canal, the vas deferens bends sharply and goes down into the pelvic cavity, descending along its side wall to the bottom of the bladder. Entering the thickness of the prostate gland, the vas deferens becomes thinner and becomes a narrow canaliculus, merging with the excretory duct of the seminal vesicle, and together with it forms a single ejaculatory duct. The ejaculatory duct, passing obliquely through the posterior part of the prostate gland, opens into the prostatic part of the urethra.

Function of the vas deferens- conduction of sperm: from the distal part of the vas deferens through the ejaculatory strait, sperm is discharged into the urethra, from there, during sexual intercourse, into the woman’s genital tract. Contraction of the wall of the vas deferens due to the significant development of muscle elements ensures ejaculation (ejaculation).
Urethra (urethra)- This is part of the male urinary and reproductive systems.
In men, the urethra is 18-23 cm long (in a state of erection of the penis - a third more, in childhood one third smaller), located both in the pelvis and inside the penis, and opens with an external opening on its head.
Throughout its entire length, the urethra has an unequal lumen diameter: narrow parts alternate with wider ones. One narrowing is located at its internal opening, another - when the urethra passes through the urogenital diaphragm, the third - at the external opening of the urethra. There are also three dilations: in the prostatic part, in the bulbous part and at the end of the urethra, where the scaphoid fossa is located. On average, the width of the urethra in an adult male is 4-7 mm.
The urethra in men is conventionally divided into three parts: prostatic (prostatic), membranous and spongy (cavernous, spongy).
Anatomically, the following sections of the male urethra are distinguished:
1. external hole;
2. scaphoid fossa;
3. penile;
4. bulbous;
5. membranous;
6. prostatic (proximal and distal areas).

Function of the urethra:
Serves to remove urine from the bladder and also to release sperm.
Scrotum- refers to the external male genital organs and is a musculocutaneous sac that contains the testicles with appendages, as well as the testicular and cord sections of the right and left vas deferens. On the inside, it is covered with a sheath of connective tissue, which forms a septum in the scrotum, dividing its cavity into right and left halves. In total, the scrotal wall consists of seven different membranes, which are also the membranes of the testicle. This structure corresponds to the structure of the anterior abdominal wall. The scrotum is connected to the latter through the inguinal canals. Normally, the right and left inguinal canals do not have a lumen, since they are filled with spermatic cords. On the outside, the scrotum is covered with thin and delicate skin, covered with hair and a large number of folds. The skin of the scrotum is also more intensely dark in color than the skin of other areas of the body.
It is noteworthy that the location of the testicles in the scrotum in this form allows them to create an ambient temperature that is an order of magnitude lower than directly inside the body. As for specifics, the optimal temperature threshold is considered to be 34.4C. It should be noted that this figure is approximate, since different people, depending on the characteristics of the organism, it may change slightly in both planes, that is, it may be slightly lower or higher.
Temperature It turns out to be preserved due to the fact that during high temperatures the scrotum lowers, and at a time when the ambient temperature is low, it is pulled towards the body. It is in this way that, in fact, it is possible to maintain a certain balance.
Function of the scrotum:
The organ functions as a sac and contains the testicles.
Penis (Penis)
At rest, the size of the penis is determined by the degree of filling of the cavernous (cavernous) bodies with blood. The corpora cavernosa, which are spongy formations consisting of many small vessels and cavities, are capable, like other vessels of the body, of responding to the action of active substances present in the blood, as well as to the influence of temperature factors. Thus, when the air temperature decreases, the vessels of the penis narrow, which leads to a decrease in blood flow into the corpora cavernosa and a reduction in the penis. As the temperature increases, a reverse reaction occurs.
Constriction of blood vessels and a decrease in the size of the penis also occurs when adrenaline is released into the blood in response to fear or another stressful situation. Therefore, it happens that the penis, which is large and “representative” during an erection, is repeatedly reduced and contracts at rest.
The size of the erect penis is limited by the tunica albuginea - a structure containing strong connective tissue, which limits the stretching of the penis during erection.
It is now believed that the level of the hormone testosterone during puberty plays a major role in the development of the penis, determining its size. At the same time, the small size of the penis (less than 8-10 cm) may indirectly indicate serious endocrine disorders associated with low production of male sex hormones.
On the other hand, a fairly large spread in the normal length of the penis (12-18 cm) can be explained by individual differences in the anatomy of the inguinal region, namely the ratio of the hidden and free parts of the corpora cavernosa and the surrounding tunica albuginea.
There is an opinion that with normal levels of sex hormones and normal development of the corpora cavernosa in different men Due to individual characteristics, the hidden part of the cavernous bodies, responsible for attaching the latter to the pubic bones with supporting ligaments and fixing the penis, is expressed differently.
However, for most men, the main importance is their own idea of the normal size of the penis, formed on the basis of personal sexual experience or the desire to be “better than others”; the average indicators, as a rule, are not taken into account by them.
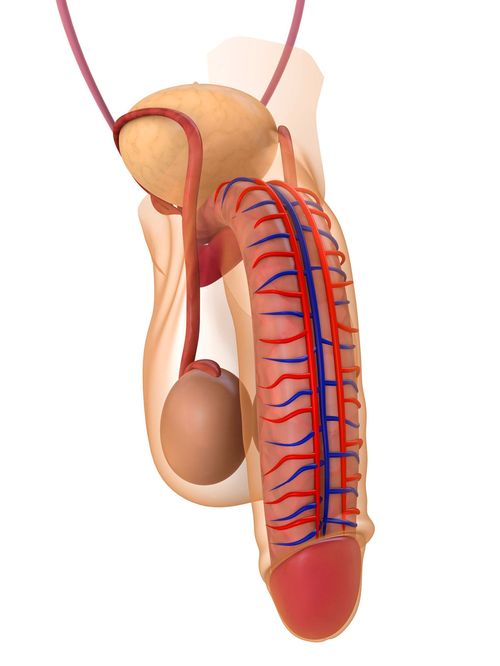
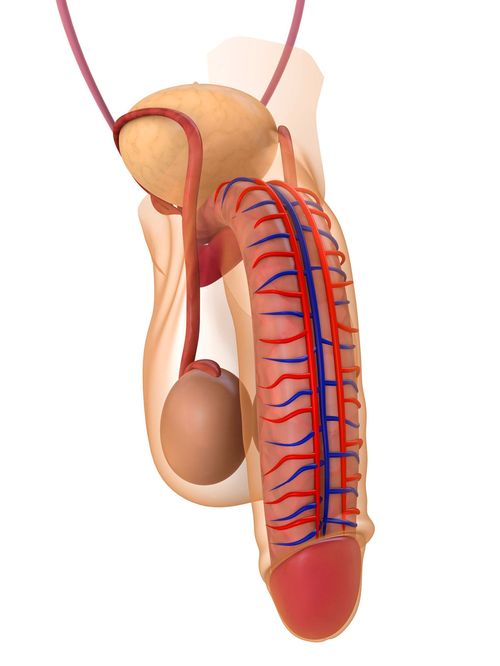
Penis:
An organ that serves to excrete urine and eject semen. It consists of an anterior free part - the body, which ends in the head, and a posterior part, attached to the pubic bones by supporting ligaments. The glans penis is divided into the widest part, the crown of the glans, and the narrowest part, the neck of the glans. The body of the penis is covered with thin, easily movable skin. There is a seam on its lower surface. In the anterior part of the body, a fold of skin is formed - the foreskin of the penis, which covers the head and then passes into the skin of the head of the penis. On the lower surface of the organ, the foreskin is connected to the head using the frenulum of the foreskin. At the top of the head of the penis, the external opening of the urethra opens, which looks like a vertical slit.
There are the root (base), body (trunk) and glans penis. The trunk is formed by two cavernous and spongy bodies containing a large number of lacunae (depressions) that are easily filled with blood. The cavernous bodies are located at the edges, the spongy body is located below, in the groove between them, along with the urethra (urethra) passing through its thickness.
The corpus spongiosum at the end of the penis ends in a cone-shaped thickening - the glans penis. The edge of the head, covering the ends of the cavernous bodies, fuses with them, forming a thickening (corolla) around the circumference, behind which the coronary groove is located. The head is covered with thin, delicate skin (foreskin) with a large number of glands that produce smegma ((sebum) - a mixture of the secretion of the sebaceous glands of the foreskin, dead epithelial tissue and moisture)
The head, like the body of the penis, contains many lacunae (gaps between tissue elements), which fill with blood during sexual arousal. In addition, it contains a large number nerve endings, which makes it most sensitive to touch. The shaft of the penis, especially its lower zone in the region of 2-3 cm from the head, is also highly sensitive. Stimulation of the penis, especially its head, leads to increased erection.
IF head:
The head of the penis is covered with delicate skin permeated with glands, and the glands maintain a certain degree of moisture on its surface. The skin of the glans is rich in nerve endings and very sensitive - much more than the penis itself.
Foreskin- this is a fold of skin that tightly fits the head of the penis. When urinating, it pulls back slightly, opening the opening of the urethra, and during an erection it completely exposes the head, stretching all the way to the corolla. The corolla is a ring-shaped fold of skin through which the head is connected to the body of the penis.
On the underside of the head is located bridle- a strip of skin connecting the foreskin to the glans. The frenulum develops during the embryonic period from the fused edges of the niche from which the penis is formed. The bridle is something like a limiter; it prevents the foreskin from moving beyond a certain point, especially during an erection. The frenulum has more nerve endings than the glans. Like the coronet, this is the most sensitive part of the penis.
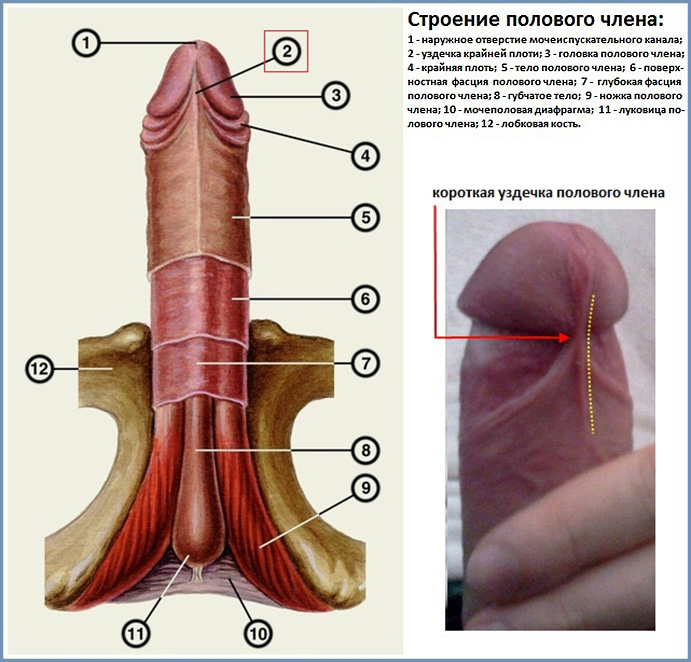
Cavernous (cavernous) body- This is the structural part of the penis. The corpora cavernosa (right and left) are cylindrical in shape and located inside the penis. To the ventral surface of the cavernous bodies, parallel to them, is the spongy (spongiosum) body of the penis.
Anatomically, the corpus cavernosum is divided into:
(1) apex (apex) - distal part;
(2) middle part;
(3) pedicle - proximal part.
In the apical part, the cavernous bodies are covered by the glans penis, which is part of the corpus spongiosum. At the symphysis pubis in the proximal part, the cavernous bodies diverge downward and posteriorly parallel to the descending (ischial) branches of the pubic bones, to which they are attached by ligaments, and are covered from above by the ischiocavernosus muscle. In the area of the symphysis pubis, the corpus cavernosum is attached to the bones using the unpaired infundibular ligament. The corpora cavernosa can be felt as ridges on the right and left inside the penis.
The corpus cavernosum consists of cavernous tissue surrounded by a tunica albuginea. Cavernous tissue has a cellular structure. Each cavity (cell) has the ability to change its internal volume by changing the tone of the smooth muscle elements (trabecular muscles) included in the structure of the cavern walls. Blood enters the caverns through arterioles radiating from the cavernous artery, located centrally inside the corpus cavernosum.
During sexual arousal, in response to the release of a mediator (NO - nitric oxide), due to the relaxation of the trabecular muscles and the muscles of the walls of the cavernous arteries, the lumen of the cavernous arteries and the volume of the caverns increase. Increasing blood flow to the cavernous tissue and filling the caverns with a larger volume of blood leads to an increase in the total volume of cavernous tissue (tumescence or swelling of the penis).
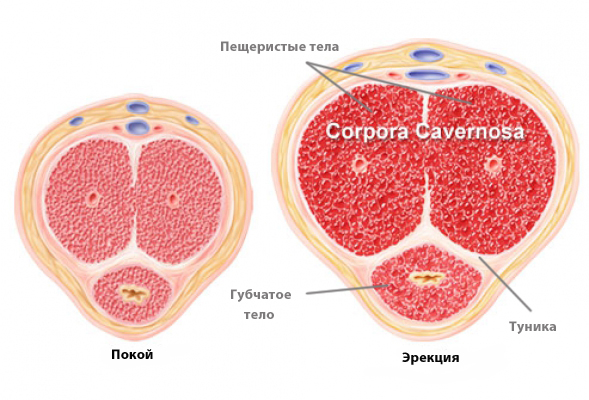
Normally, the outflow of blood from the cavernous tissue occurs through the venous plexuses located directly under the tunica albuginea. When the venous plexuses are pressed to the tunica albuginea due to an increase in the volume of cavernous tissue during tumescence (the basis of the veno-occlusive mechanism), the outflow of blood from the cavernous bodies decreases, leading to the appearance of a hard erection.
At the end of sexual activity (usually after ejaculation), the release of norepinephrine, a sympathetic transmitter that increases the tone of the trabecular muscles, leads to the disappearance of an erection (detumescence) in the reverse order to the appearance of an erection. Insufficient blood flow to the cavernous bodies, excessive outflow of venous blood from the cavernous bodies, damage to the nerves that conduct signals for the appearance of an erection, as well as damage to the cavernous tissue leads to a deterioration in the quality of erection, up to its complete absence
Main function of the corpora cavernosa- ensuring erection of the penis (increase in size and hardening of the penis during sexual arousal).
Corpus spongiosum (spongiosum):
The corpus spongiosum is located on the lower surface of the penis in the groove between the cavernous bodies. The corpus spongiosum is formed by fibrous tissue, which also contains cavernous tissue, which fills with blood during erection, just like the cavernous bodies. The urethra passes through the thickness of the corpus spongiosum to excrete urine and sperm. The corpus spongiosum is also covered with a separate thin tunica albuginea. The anterior and posterior ends of the corpus spongiosum are expanded and form the head of the penis in front, and the bulb in the back.
The corpus cavernosum and spongiosum, with the exception of the head, are surrounded by a common deep fascia, which is covered by the superficial fascia. Blood vessels and nerves pass between the fascia.
Function of the spongy body:
It is a conductor and protector of the urethra. And together with the corpus cavernosum of the corpus spongiosum, it forms the erectile tissue of the penis, which participates in the erection of the penis.
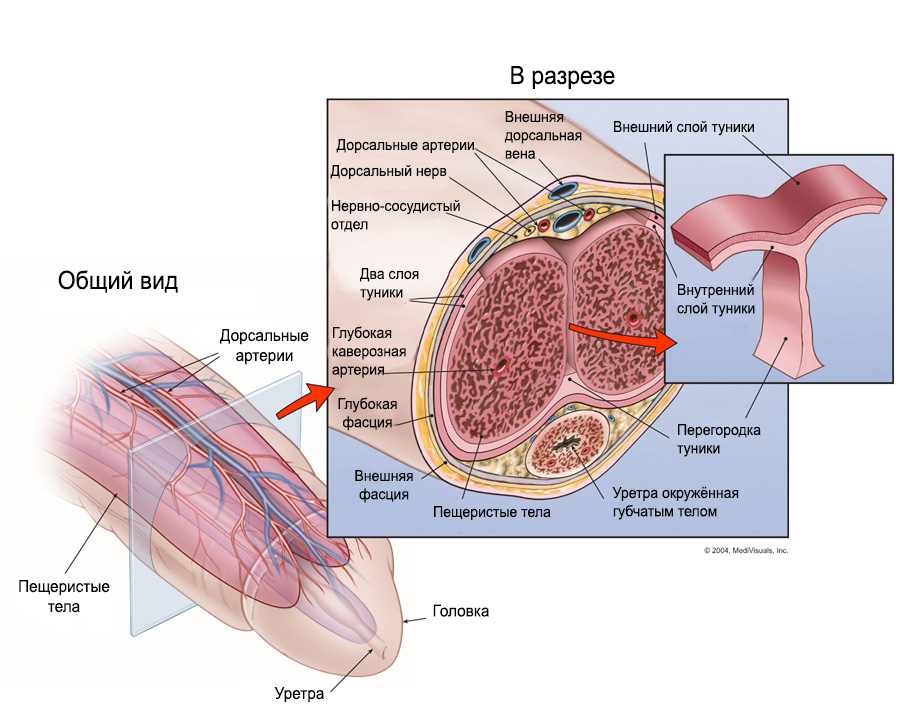
Tunica albuginea of the cavernous bodies (tunica):
The tunica albuginea of the corpus cavernosum is the case for the cavernous bodies. During an erection, the tunica albuginea stretches evenly in different directions, provides symmetrical enlargement of the penis. Congenital disorders of the elasticity of the tunica albuginea, scar changes after injuries to the penis and the formation of fibrous plaques on the tunica albuginea in Peyronie's disease can lead to curvature of the penis during erection.
The tunica albuginea is a complex, complex structure consisting of 2 layers - internal and external. The inner layer consists of circularly oriented collagen fibers interwoven into the cavernous tissue. They form the median septum and intracavernosal internal supports, forming chords between 2 and 6, 6 and 10 o'clock on the conventional dial.

The outer layer consists of large longitudinally located fibers, represented by large individual bundles from 4 to 5, from 7 to 8 and from 11 to 1 o'clock on the conventional dial. This layer also forms the ventral thickenings - triangular structures located at 5 and 7 o'clock. Between them runs a ventral groove in which the corpus spongiosum is located. The small number of collagen bundles between the ventral thickenings allows the corpus spongiosum to increase in size without limitation during erection.
On the dorsal side, the longitudinal bundles of the outer layer are connected into structures called dorsal thickenings. Proximally, they are located at 11 and 1 o'clock on the conventional dial and are attached to the internal pubic process. Between them runs a dorsal groove in which the neurovascular bundle lies.
The proximal dorsal thickenings merge into a single structure at 12 o'clock and continue into the glans penis. Laterally, the fibers of the outer layer are woven into the suspensory ligament and pass through it until they connect with the adjacent ischiocavernosus muscle.
Another component of the tunica albuginea is elastic fibers, which form a mesh structure in both the outer and inner layers.
Stretching the tunica albuginea (tunica) of the cavernous bodies helps to increase the length and girth of the intestinal tract.
Function of the tunica albuginea:
Limits the size and stretch of the penis during erection, thus giving it hardness.
Bundles:
Anterior to the pubic symphysis, the corpus cavernosum and corpus spongiosum come together and are attached to it by a suspensory ligament, which encircles the base in a loop with a movable sling-shaped ligament. At this point the fixed part of the penis ends, which passes into the movable pendulous part.

By stretching the inverter and hanging loads on it, we additionally influence the ligaments, the stretching of which helps to increase the length of the inverter due to the hidden part.
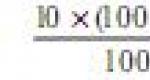
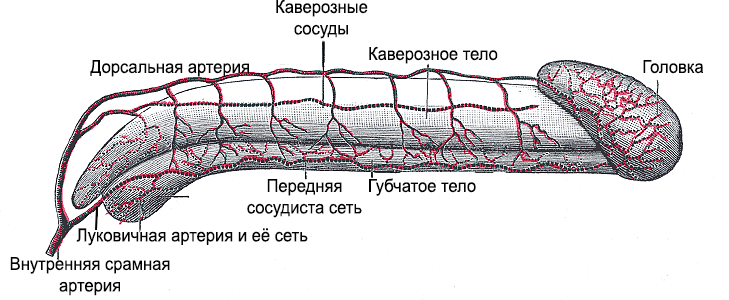
Blood supply:
The blood supply to the penis is carried out through the deep and dorsal arteries of the penis, which are branches of the internal pudendal artery.
Venous blood from the penis flows through the deep dorsal vein into the cystic venous plexus and through the deep veins of the penis into the internal pudendal vein. 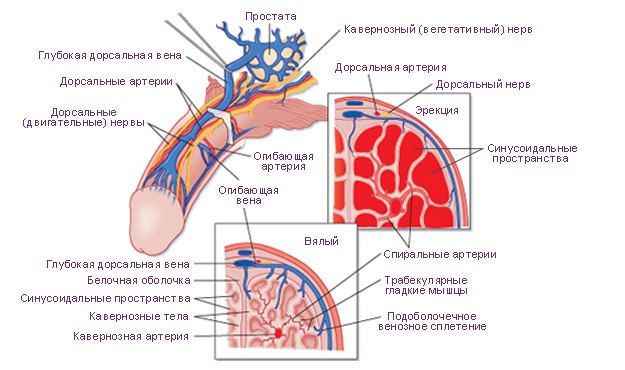
![]()
By doing vascular exercises, we help to strengthen and increase the vascular-capillary network, which leads to an increase in the girth of the infarction.
Innervation (nerves):
The sensory nerve is the dorsal nerve of the penis (a branch of the pudendal nerve). The sympathetic nerves come from the inferior hypogastric plexuses, and the parasympathetic nerves come from the pelvic splanchnic nerves.
Penile muscles:
Most men believe that a penis is completely external organ. But when you look at yourself naked in the mirror, you are only seeing half the picture. The other half of your penis is inside your body and is called the internal penis.
Your inner penis is surrounded by the muscles of the pelvic diaphragm - the bulbospongiosus (LG) muscle and the ischiocavernosus (SP) muscle. Together, these two muscles are responsible for pumping blood into the penis, causing a chain reaction of sorts that leads to an erection. The health of these muscles greatly affects the health of your genitals, which is why you should always perform Kegel exercises, which are aimed at stimulating these muscles.

The inner penis and pelvic diaphragm muscles can be felt by touching the perineum - the place between your testicles and anus.
1. bulbospongiosus muscle, covers the bulb and the posterior part of the spongy body - starts from the tendon center of the perineum and is fixed to back surface cavernous bodies and the fascia of the penis; - as a result of muscle contraction, the outflow of venous blood from the cavernous bodies during erection is hampered, sperm is squeezed out of the urethra during orgasm and the last drops of urine during urination
2. ischiocavernosus muscle, paired - begins posteriorly from the root of the cavernous body and the sacrotuberous ligament; the tendon is woven into the tunica albuginea of the corpus cavernosum; - when contracted, the muscle presses the root of the corpus cavernosum to the bone, straightens the penis, and compresses its dorsal veins.
There are also smooth trabecular muscles inside the penis itself (IF muscle). Smooth muscles are located inside three vaulted cavities (cavernous and spongy), and the shape and size of your penis depend on them. When the smooth muscles are contracted, the penis is not erect. When the smooth muscles relax, the penis fills with blood and an erection occurs.
There are many differences between men and women, and they are most pronounced in the genitals. In guys, the reproductive and urinary functions are performed by the penis. The structure of the penis is the same in all men, unless there are deviations from the norm. Now let’s look at what this organ consists of, as well as what processes it is responsible for.
Considering the structure of the male penis, we can distinguish three main components: the base (also called the root), the body and the head. The base is firmly attached to the pubic bones. The widest part can be called the head area, but the neck, on the contrary, is considered the narrowest.
The shaft of the reproductive instrument is formed from the cavernous and spongy bodies. They contain a large number of depressions that can be filled with blood fluid. The bodies, called cavernous bodies, are located along the edges of the penis. And the spongy is located below, in the groove between the cavernous ones. Its diameter is approximately 1 cm.
The structure of the male genital organs includes the head, and it is at the end that the spongy body turns into a cone-shaped thickening. This part is covered with cavernous bodies, from which the corolla is formed (it is a thickening around the circumference). Immediately behind it there is a coronal groove.
The skin of the head is very thin and delicate, it has many glands that produce smegma. There are nerve endings in this area, due to which it becomes very sensitive to touch. The trunk of the organ, especially the area near the head, has a similar property. At the very top of the penis there is a small hole through which urination is performed and seminal fluid is released. This channel is a hollow tube, the end of which is closed.
If the structure of the male penis is the same in all people, then appearance may vary. It all depends on individual characteristics and genetic data. As a rule, in a state of erection the penis is slightly curved, but when at rest it appears straight.
Some representatives of the stronger sex who have recently entered adolescence may notice a small amount on their skin. They shouldn't be painful. This can be explained by the fact that the penis has sebaceous glands. If a person adheres to the rules of personal hygiene, then their work will be invisible. But, if the glands become clogged due to hormonal changes or poor care, then their size increases significantly.
To quickly enlarge the penis, our readers recommend Titan Gel Cream. This is a natural remedy that helps to enlarge your penis by 3.5 cm in just 2 weeks! Titan Gel contains only natural ingredients with maximum effectiveness. Due to its composition, the drug is absolutely safe, has no contraindications or side effects.
The structure of the male genital organs allows for the presence of moles or hairs on the surface. However, if other formations appear, for example, or a growth, then you should contact a specialist. Normally they shouldn't be there.
Structure and anatomy of the penis
About the foreskin
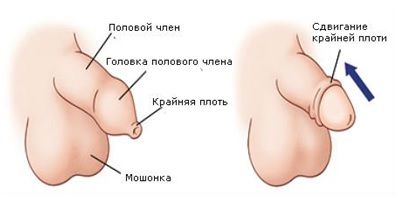 In the area of the head of the penis there is a thickening of the skin that looks like a fold. It is called the foreskin. At the bottom there is a connection using a bridle. It is she who does not allow the flesh to move beyond a specific border.
In the area of the head of the penis there is a thickening of the skin that looks like a fold. It is called the foreskin. At the bottom there is a connection using a bridle. It is she who does not allow the flesh to move beyond a specific border.
It is worth understanding that newborn babies have physiological phimosis– the head cannot be opened. But with age, it begins to become naked painlessly and easily. If this does not happen, then this is a reason to consult a doctor.
Some ethnicities consider it normal to have the foreskin surgically removed. As a rule, this is due to the climate, as well as the fact that inflammation often occurs due to this part of the organ. Religion also comes into play; in some faiths, circumcision is a mandatory action.
 Having examined the structure of the penis, it should be separately noted that it cannot normally perform its function without a blood supply. It reaches the organ through a group of vessels. There are anterior scrotal arteries that arise from the external genitalia. There is also a dorsal artery, which originates in the internal pudendal artery. It is these structural elements that provide blood to the outer part of the organ.
Having examined the structure of the penis, it should be separately noted that it cannot normally perform its function without a blood supply. It reaches the organ through a group of vessels. There are anterior scrotal arteries that arise from the external genitalia. There is also a dorsal artery, which originates in the internal pudendal artery. It is these structural elements that provide blood to the outer part of the organ.
As for the internal formations, their blood supply system consists of the deep and dorsal arteries. It is also worth mentioning the outflow of blood fluid. It is performed by the deep vein and the vein of the bulb, which pass into the vesical plexus, and then into the internal genital vein.
It is thanks to blood that the penis is able to become erect and perform the function of fertilization.
What you need to know about size?
Structure male penis All people have the same size, however, the size is individual. Each person has his own, but are there certain standards? We can say which parameters are considered normal and which deviate from the generally accepted ones.

What sizes are there:
- As a rule, if the reproductive organ is in a calm state, then its length will be from 5 to 10 centimeters. We are talking about a sexually mature person.
- When erect, the length increases significantly. The average is considered to be 14-16 cm. However, if the parameters are at around 10 cm, then this is also in the order of things, and not a deviation from the norm.
- An organ that is 18 cm or longer is considered large. This happens quite rarely.
- If during an erection the length is no more than 8 centimeters, then this will already be considered a pathology. In this situation, you should consult a doctor and, together with a specialist, consider what can be done in this case. Penis enlargement surgery may need to be considered.
- There is also such a deviation as micropenis. In this case, the length of the penis is up to 2 centimeters.
If we talk about the diameter, then on average it is from 3 to 5 centimeters. But deviation is possible, both upward and downward.
At birth, in boys, the length of the organ is usually from 2 to 5 cm. However, by puberty it increases to 6 cm. In subsequent years, until about 17 years old, the penis grows rapidly. It also continues to increase until age 25, but slowly and almost imperceptibly.
There is an opinion that the size of the penis is directly related to the size of the nose or fingers. However, such guesses have not received scientific confirmation. We can only say that there is a connection with human growth.
About the functions
The purpose of the penis is clear to most people, but it’s worth looking into it again. Men's reproductive system directly involved in the production of germ cells, which are called sperm. In the future, they participate in the fertilization of the egg, which leads to the birth of a child. Manhood directly involved in the release of seminal fluid into the vagina during intercourse. This is what subsequently leads to fertilization. The organ is also responsible for the production of sex hormones.
As already mentioned, active formation of sperm occurs in mature men. They are updated approximately every two months. If a man has bad habits, the quality of the seminal fluid will deteriorate. For this and other reasons, it can be observed, which leads to difficulty or impossibility of conception. Sometimes it can be cured, but sometimes you just have to accept infertility as a fact.
The reproductive system includes the testicles, which are a paired oval-shaped organ. In size they can be compared to a walnut. They are located in the scrotum. Considering that they have many nerve endings, the testicles are extremely sensitive to any influence.
The testicles are directly responsible for the production of seminal fluid. It occurs in the seminiferous tubules. This organ also manages hormones, directly testosterone.
As for the scrotum, it looks like a leather pouch that is located right near the base of the penis. The skin is quite delicate, with sparse hairs. The scrotum is divided into two parts by a septum. Its size can change depending on the temperature.
If the body functions normally, a man will be able to perform his sexual function. However, if pathologies exist, problems may arise with sexual intercourse, conception, and the production of hormones and sperm. That is why, in case of any deviations, you should contact a specialist. Moreover, pathologies can be detected both in childhood and in adulthood.
What diseases are there?
It is useful to know not only the structure of the glans penis and the reproductive system itself, but also existing diseases. There are a lot of ailments, and they can have different etymologies. Considering the number of diseases, let's look at the most common ones.
 If the problem is not congenital, then, as a rule, its appearance can be provoked by low physical activity, poor environmental conditions, decreased immunity, promiscuity or lack thereof. Injuries and surgery can also lead to problems.
If the problem is not congenital, then, as a rule, its appearance can be provoked by low physical activity, poor environmental conditions, decreased immunity, promiscuity or lack thereof. Injuries and surgery can also lead to problems.
If we talk about infectious diseases, their symptoms are in many cases clearly visible. Among the signs:
- Burning and itching.
- Unnatural discharge.
- Pain, redness, swelling of the penis.
- The appearance of skin rashes.
Sexually transmitted diseases are caused by bacteria, fungi, viruses and protozoan microorganisms. Most often they are transmitted through sexual contact, less often when sharing the same personal hygiene item with a sick person.
There are many types of diseases, and among them the leader is thrush, which occurs in both sexes. Patients are also often diagnosed with syphilis, gonorrhea and chlamydia. To diagnose, you should take tests and undergo a professional examination. If the disease is not treated, serious consequences, including infertility and death, are possible.
If we talk about pathologies, then a representative of the stronger sex can. In this case, a person is able to participate in sexual intercourse, but his sperm are inactive. As a result, fertilization is impossible.
 Among the inflammatory ailments, balanoposthitis and vesiculitis can be noted, which manifest themselves as unpleasant sensations. If left untreated, a man may become infertile.
Among the inflammatory ailments, balanoposthitis and vesiculitis can be noted, which manifest themselves as unpleasant sensations. If left untreated, a man may become infertile.
We often hear about impotence, but it can occur not only in old age, but even at 30 years of age and earlier. It can be triggered by either a mental factor or an unhealthy lifestyle or disease. As a result, a man has no sexual desire, he cannot participate in sexual intercourse, there is no orgasm and satisfaction. Treatment is possible with timely consultation with a doctor.
There are other pathologies, for example, ejaculation disorders, paraphimosis, cystitis, prostate adenoma, delayed ejaculation, etc. If a man suspects certain deviations from the norm, he should immediately see a doctor and under no circumstances self-medicate.