Contrast agents may be administered. MRI and CT with and without contrast - what is the difference in examining the brain, are there any contraindications
Contrast agents, the basis of which is iodine, are used for a thorough examination of blood vessels, detection of malignant and benign neoplasms, when diagnosis without the use of contrast does not give the desired result.
For example, the answer to the question - why contrast is needed is given by tomography of the adrenal glands, which will be difficult to distinguish using a native study, but using contrast enhancement, they become visible.
The administration of an iodine-containing drug is carried out by three methods:
- Orally;
- Through the circulatory system (intravenously);
- Rectally (through the rectum).
Why do you need contrast in computed tomography?
Purpose contrast agent is based on the precise separation of healthy and pathological areas of the human body, differentiation of organs using a stronger signal received from the circulatory system. A preliminary creatinine test before CT is necessary to exclude renal pathology. The drug is excreted through the urinary system.
In the image, the area of contrast accumulation is highlighted in white, which makes it possible to clearly see individual sectors of the area under study and make the correct diagnosis.
Preparing for the administration of a contrast agent
Before performing a contrast-enhanced CT scan, some preparation will be required.
Firstly, the procedure is done on an empty stomach.
Secondly, you need to follow a diet - give up fatty, spicy foods, remove flour and smoked products from your diet. Porridges and light soups are perfect. You need to drink as much fluid as possible.
Thirdly, you should not use alcoholic drinks 2-3 weeks before the examination.
You will also need to quit smoking at least 24 hours before.
If you are allergic to iodine, you must inform your radiology doctor before starting a CT scan with a contrast agent.
Name, types of contrast agents for CT
Substances used for contrast enhancement, can be divided into two main groups:
- Gaseous forms (air contained in the room or inert gas);
- Preparations based on iodine.
The first method is more often used when scanning hollow organs in order to identify symptoms and signs of diseases after stretching the walls with air. This type is used extremely rarely.
The second method is more suitable for examining blood vessels and detecting malignant and benign neoplasms. Preparations containing iodine are divided into non-ionic and ionic.
Non-ionic form - substances of a new generation - ultravist, unigexol, omnipaque, ioversol, iopromide. Ionic composition is a more obsolete form. Representatives of this type include urografin, metrizoate, diatrizoate, ioxaglate.
Contrast agents with iodine, without iodine
Drugs to enhance during conduction computer diagnostics can be divided into iodine-containing - consisting of iodine salts and substances without the presence of iodine, the main element of which is barium sulfate. The latter are insoluble in water, their contact with body tissues is minimal.
The first group is divided into water-soluble, intended for parenteral use (bolus form of enhancement, angiography) and fat-soluble, having a high viscosity, used for hysterosalpinography, sialography.
Based on their composition, iodine-containing preparations are divided into ionic and non-ionic. Preference is given to the second group due to the minimal incidence side effects.
The places where contrast agents are injected are the peripheral (elbow) and subclavian vein (using a central catheter). For injection, use an automatic injector or do the injection manually, but the first method is preferable.
Each iodine-based contrast agent is distinguished by its main parameter - “strength”, which reflects the quantitative indicator of the active substance. For example, Ultravist-300, which contains iodine in the amount of 300 mg per 100 ml of product, is less “strong” than Ultravist-370 containing 370 mg of iodine and requires increased doses for a clearer scan.
Composition of contrast agent for computer scanning
 For example, let’s look at the drugs: ultravist, which is a nonionic iodine-containing drug, and urografin, an ionized form.
For example, let’s look at the drugs: ultravist, which is a nonionic iodine-containing drug, and urografin, an ionized form.
Ultravist: active ingredient – iopromide (replacement iodine); excipients - trometamol, sodium calcium edetate, hydrochloric acid, water for injection.
Urografin: active ingredients – meglumine amidotrizoate, sodium amidotrizoate; excipients – sodium calcium edetate, sodium hydroxide, water for injection.
How intravenous contrast is done during a computer scan - enhancement phases
The administration of contrast using the bolus method occurs intravenously under high pressure and with high speed(about 5 ml/s), which allows you to see the condition of the vein - how much load it can bear and change the injection rate, focusing on the person’s condition and the quality of diagnosis.
It is first necessary to install a catheter with a wide lumen - with a pink, green, gray, which is a required element. In products with a narrow lumen, the flow rate of the injected substance will be very high, and the vessel may rupture.
CT with contrast is required precise definition doses of the administered element for qualitative examination. Products containing 370 mg of iodine are subject to the following condition: 1 ml of contrast corresponds to 1 kg of weight. There are a number of exceptions to the rule:
- When scanning the vessels of the head and neck, it will be enough to use 40-50 ml of contrast agent;
- Abdominal and pelvic examination allows the use of 60-80 ml (possibly more, depending on weight);
- With tomography chest(to exclude pulmonary embolism) 50-70 ml is used;
- Examination of the extremities – 50-60 ml.
Such centers issue a conclusion after the end of the procedure, with which you can contact your doctor and prescribe treatment without wasting time.
Computed tomography (CT) is widely used in the world for diagnosing a number of diseases, allows identifying pathology in the early stages of development and is more informative than standard x-ray and ultrasound methods. Contrast tomography is considered a high-tech method, and its purpose must be strictly justified.
What is the difference between standard computed tomography and CT with contrast? Indications and contraindications. Types of contrast agents
The CT method was developed in 1972 by Godfrey Housefield and Allan Cormack, who was awarded the Nobel Prize. Its essence is to obtain a series of layer-by-layer images of the internal structures of the body using X-rays.
Tomography allows you to examine the entire organ, tissue, vessel, and identify the presence of pathological formations. If it is necessary to clearly separate healthy tissue from damaged tissue, contrast is used.
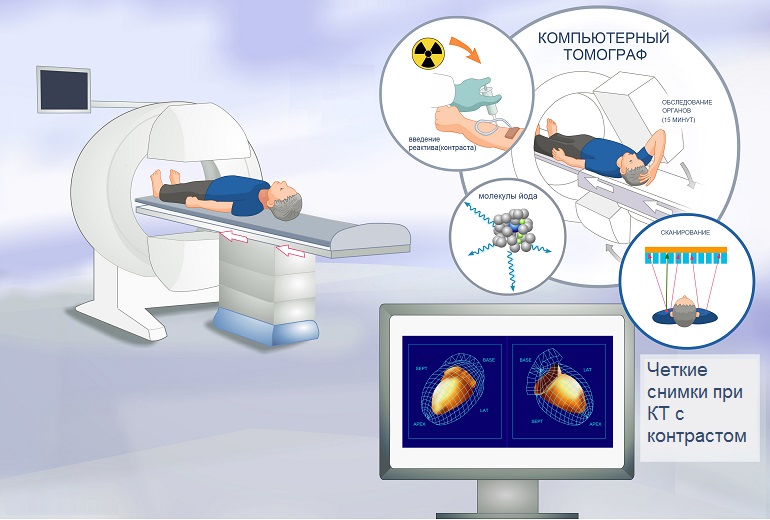
CT machine
Indications for examination with contrast agent:
- suspicion of a massive process: tumors of the brain and spinal cord, lymphoma;
- damage to parenchymal organs abdominal cavity(hepatoblastoma, carcinoma, pancreatic necrosis);
- pathology of retroperitoneal organs (nephroblastoma, neuroblastoma);
- damage to the hollow organs of the abdominal cavity (intestines, stomach);
- bone tumors (sarcomas);
- damage to joints and ligaments;
- vascular anomalies.
Important! CT scan with contrast helps to differentiate benign and malignant processes, determine the required extent of surgery, if one is planned, and exclude vascular pathologies.
Like any study, CT with contrast has a number of contraindications:
- allergic reactions to iodine;
- uncompensated diabetes mellitus;
- bronchial asthma;
- renal failure;
- pathologies of the thyroid gland;
- claustrophobia and mental disorders, in which the patient is unable to control himself;
- pregnancy;
- severe obesity, since the device has weight restrictions.
Before prescribing a CT scan, it is important to find out the medical history and conduct a biochemical blood test to assess functional state body. If there are absolute contraindications, the study should be cancelled.
Classification of contrast agents
Computed tomography can be performed with two types of contrast: fat-soluble and water-soluble. Both drugs are based on iodine, which increases the intensity of the image and does not have a pronounced toxic effect on the body.
Water-soluble contrast (for example, Urografin) is used to evaluate the kidneys, urinary tract, blood vessels, and abdominal organs. Fat-soluble (for example, Iodolipol) is limited in use due to its high viscosity; it is used for intracavitary administration (excluding fistulas). Water-soluble contrasts are preferred for use because they:
- give less allergic reactions;
- quickly distributed in the vascular bed;
- can be administered intravenously and orally (by mouth).
Alcohol-soluble and insoluble contrasts are practically not used today.

Water-soluble contrast Urografin
CT technique. Routes of drug administration
The study lasts 50-60 minutes. The patient must be hungry and all jewelry and removable metal items must be removed. When examining the abdominal organs, the day before you should take drugs that reduce gas formation (for example, Espumisan). You must lie still, layer-by-layer sections must be clear. First, a native CT scan is performed, that is, without the introduction of contrast. Then the drug is injected and after a certain time, which depends on the area being examined, images are taken again.
There are several ways to administer a contrast agent:
- Oral – the drug is drunk through the mouth. This technique is used in diagnosing pathology of the hollow organs of the abdominal cavity (intestines, stomach).
- Intravenous can be administered manually or by bolus. In the first case, the medical worker himself administers the substance through a catheter. In this case, it is impossible to accurately adjust the speed. At computed tomography with bolus contrast, a catheter is installed in the ulnar vein and an infusion pump is connected to it (a special device - an electronic dropper). The time and required amount of contrast are set. Standard scanning is carried out at 30, 60 and 180 seconds.
- Into the lumen of the cavity. This method is used to study Bladder and the presence of pathological formations (fistulas, diverticula).

Standard intravenous contrast administration
The cost of CT with bolus contrast is slightly higher. But standard intravenous administration of the drug is unacceptable for angiography and coronary angiography. Doctors take these nuances into account when prescribing a test.
Adverse reactions
In rare cases, side effects may develop. The most common ones include:
- dizziness;
- nausea and vomiting;
- arterial hypotension;
- allergic rash, Quincke's edema;
- bronchospasm;
- shortness of breath, tachycardia.
Remember! Throughout the study, the patient can communicate with the doctor and, if necessary, tell him about his poor health. In general, the procedure is painless and safe.
Special methods of computed tomography with contrast. Differences between CT and MRI
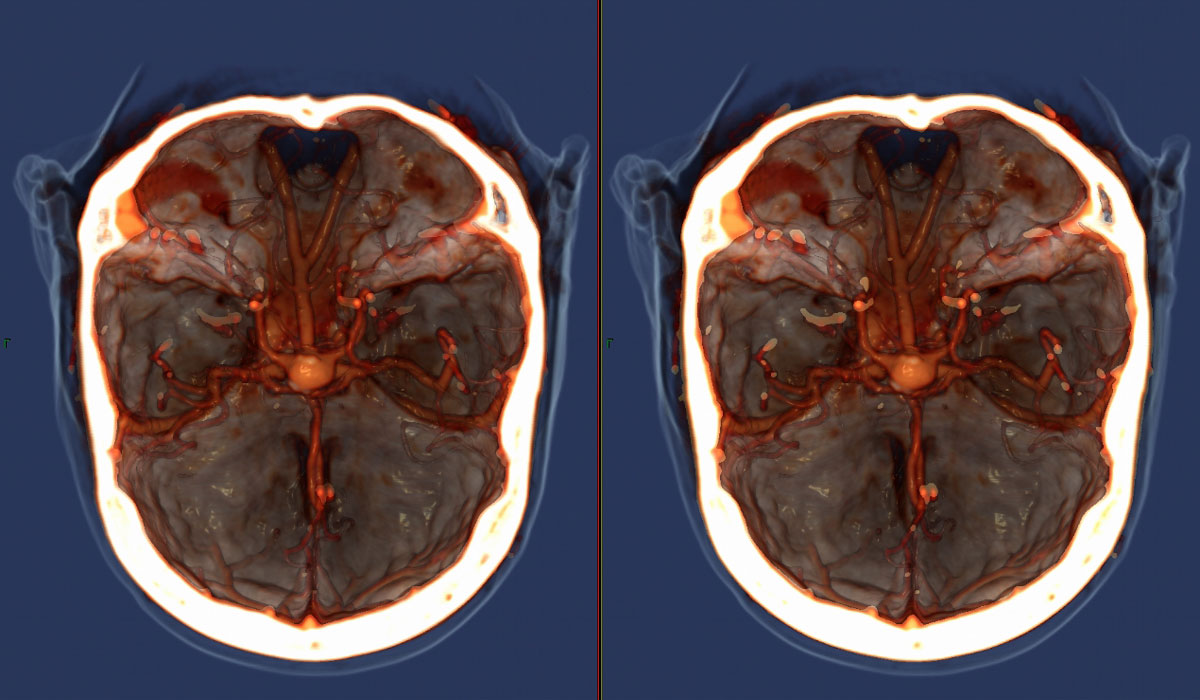
CT angiography is widely used in vascular surgery and cardiology. After a bolus injection of contrast and obtaining a series of layer-by-layer images, a three-dimensional image the entire vascular network of the body or a specific organ. This method is important for identifying blood clots, aneurysms, hemangiomas and lymphangiomas, and allows planning complex heart surgeries.
You can view the result of CT angiography of the brain in the video:
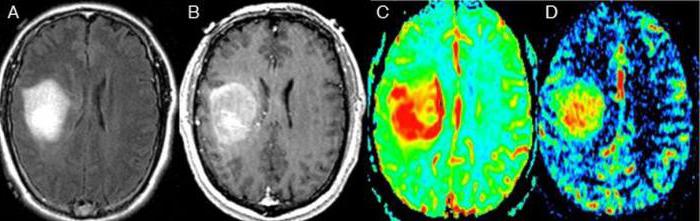
Another method is CT perfusion. It is used to evaluate the brain. Allows you to examine the structure of the brain and detect pathological formations, diagnose TBI (traumatic brain injury), stroke, and features of the blood supply to a brain tumor at the stage of therapy and before it begins.
What is MRI?
Many patients are interested in the question of how computer and magnetic resonance imaging differ and whether one method can be replaced by another. And the differences are as follows:
- Operating principle: CT uses X-rays, MRI uses a strong magnetic field.
- Use of other contrast agents. Magnetic resonance imaging uses gadolinium. This drug does not have a cross-allergy to iodine, which means that MRI is allowed in patients for whom CT with contrast is prohibited.
- MRI for vital reasons can be performed during pregnancy, unlike CT.
- MRI better visualizes soft tissue (brain, muscle tissue).
Gadovist (contrast used in MRI)
Both methods are specific and informative. Only a doctor can decide which one is better and indicated for a particular patient.
Conclusion
CT is a modern and informative method for diagnosing a number of diseases. Like any study, it has indications and limitations. If you take the necessary laboratory tests before the procedure and tell the doctor about your illnesses, there will be no side effects, and the diagnosis will be correct.
Computed tomography has been an innovative advancement that has expanded the capabilities of medicine. Many pathologies occur hidden, a person does not feel abnormalities. This is a feature of the body itself: to try to protect itself with reserve reserves and defense systems. There is already an anomaly, but the body carefully suppresses its consequences. And only when the resources have been exhausted and the pathology has become significant, a person feels changes in health based on the symptoms shown. A contrast agent for CT increases the capabilities of the device, making the diagnosis more accurate.
Of course, the capabilities of radiography were previously used. But they were limited by the lack of color. When a standard photograph is taken, it is like a photocopy. The general areas of the organ are visible, and the lesions are noticeable. But these are already serious stages, the treatment of which is difficult. And it is impossible to say that such images are insufficient for studying the brain, but they are enough for the kidneys. When diagnosing, the main goal must be achieved. And this task is to identify violations before they are fully formed and begin to progress.

CT scans are usually done with iodinated contrast material.
Contrast is not always used, since CT is an informative diagnosis and often the usual form is sufficient. However, after the picture is displayed on the monitor, the specialist evaluates the result. If upon examination there is a suspicion of neoplasms or cancer, contrast is added. Even if the fear is not confirmed, experts understand that they cannot make a mistake right now. Simply because if the inclinations are not detected now, the next time the person will come with a severe pathology. Medicine has always focused not on treatment, but on preventing the development of diseases.
At other times, it happens that an organ cannot be assessed, even using tomography. CT scan is not Magic wand, the device must sense the organ. But sometimes extraneous factors interfere or the presence of a significant fat layer. When conducting studies such as ultrasound, it is difficult to assess the condition of tissues if the layer is too large. Thus, a CT scan of the kidneys sometimes requires the administration of a contrast agent, especially if a puncture is performed or drainage or catheters are installed.
CT method
Computed tomography has much in common with MRI, so they often replace each other. But MRI has wider possibilities, but this affects the cost of the procedure, so not all patients can afford it. Thus, a CT scan of the kidneys has an approximate cost of 3,000 rubles, while an MRI of an organ already starts at 5,000 rubles with a full transcript.
The essence of the tomography method is to evaluate the organ’s response to the received rays. Unlike a simple x-ray, the result will be strictly layer-by-layer, which is critical for making a diagnosis. During a CT scan of the kidneys or lungs, the specialist evaluates tissue density, since it is different. For example, bones and tissues receive radiation in completely different ways: the former absorb, the latter transmit. This is especially important for CT scans of the brain, where there is mixed tissue.
The toxicity of the contrast agent is minimal.
During the procedure, the contrast agent is administered only by the specialist himself. If the patient has diseases or limitations that exclude such techniques, the specialist needs to voice them before administration. Especially if there are problems with the kidneys, since substances are excreted through the urinary tract. The reagent can remain in the body for a certain time, then it must leave the body. Kidney disease, especially kidney failure, may not allow this process to occur in a timely manner and without consequences.
When the rays reach an organ, be it a CT scan of the kidneys or another organ, the specialist evaluates the reaction to them. But it gets the result in dark-light colors after processing with programs. Sometimes, especially when an abdominal CT scan involving multiple organs is performed, the response of a single organ or site needs to be assessed. Then a substance is injected in order to highlight the desired area. The patient takes the reagent orally either all at once or gradually.
But substances can be administered either rectally or intravenously. Application and method of administration are selected according to the situation. Thus, during CT scanning of the intestine, it is often administered rectally, which is safer. But it depends on what exactly needs diagnosis, because the intestine consists of several sections.
When is computer diagnostics prescribed?
In general, there are no restrictions for tomography; absolutely any organ can be viewed in this way. Its application, however, later than others, was also found in ENT practice. CT scans of the brain have been done for a long time, but the opportunity to use a tomograph for ENT organs has appeared not very long ago. Even now, CT scanning of the nasal sinuses or frontal lobes is only possible on a hospital basis, if we talk about municipal clinics. Specialists in this profile have long proven the danger of untimely diagnosis in acute sinusitis/otitis.
In practice, tomography, even for the head, is not always prescribed. Most often, when an ultrasound does not produce results or is not possible. The organ also matters. Thus, a CT scan of the abdominal cavity will be more informative than an ultrasound scan. If the intestines are being examined, then a CT scan of the intestines can be replaced by a colonoscopy and vice versa. Colonoscopy is as informative as a tomograph. But it has advantages:
Kidney CT is often prescribed for symptoms of urinary system diseases. There is an ultrasound, but it will provide little information for diagnosis. There are several cases when a CT scan with a contrast agent may be prescribed:
A CT scan of the lungs requires a contrasting element, albeit a dense organ. But only contrast will allow you to better see the entire respiratory system. Compared with an ultrasound of the lungs, the tomograph provides more information. You also need to take into account the special connection with the heart. Sometimes it turns out that because the patient has complaints. But we need to pay attention to the condition of the lungs and cardiac activity; the health of this organ is important. Thus, the presence of a cough does not always indicate lung involvement. This could be a heart pathology with the same variable.
Contraindications
Contraindications apply not only to examination of the abdominal cavity. For some unknown reason, some patients believe that the reagent is accumulating in the abdominal cavity. An erroneous and incorrect belief, since the peritoneum does not accumulate anything. If there are no restrictions, the product used is removed quickly. Even with functional kidney damage, substances leave the body.
However, there are several restrictions and these contraindications must be followed:
Contraindications also apply to pregnant women; for breastfeeding women there is a temporary restriction. This is due to the fact that barium or iodine is used for contrast. Barium passes into milk and through the placenta. Therefore, for a nursing mother, you need to stop feeding for a day. But pregnant women should generally choose a different diagnostic method.
It is critical to notify the physician of the restrictions before administration. Even if there is an allergy to other substances, a specialist should know. Before administering a substance, a tolerance test is carried out. But more often it is only the barium itself, but iodine is not always possible to determine. The doctor cannot know what levels of iodine are in the blood if there are no tests. Only the patient himself knows this. If there are no thyroid diseases, you need to remember how iodine is absorbed during normal use. For example, make an iodine grid on an area of skin and evaluate the absorption rate. A primitive test and simplified, but sometimes it helps.
A tolerance test is always done in order to exclude the main consequence: anaphylactic shock. If there is a history of impaired renal function, you should discuss this with your doctor before the procedure. It is important to understand: a CT specialist is not an attending physician; he cannot fully assess the patient’s condition. Only your treating specialist can determine the advisability of a CT scan itself, so that the tissue does not accidentally accumulate anything in itself and remove contraindications.

The contrast agent is also contraindicated during breastfeeding.
If there is a ban on CT
If limitations are identified, then this computer study will completely replace MRI. The basis of MRI is completely different; different techniques and other drugs are used. The preparation is practically no different. General recommendations for both studies are identical:
- remove all metal jewelry;
- lie motionless during the process;
- follow the radiologist's commands.
The advent of the use of computed tomography has simplified diagnosis. The variety of contrast agents for modern CT scans expands the horizons in terms of treatment. In fact, this is a chance for many patients to restore health and find out about the disease in time. However, you need to understand that this is only a method of identifying the disease. It can be used to monitor the effect of therapy on pathology, which helps to adjust treatment for effectiveness. But the final result of treatment will depend only on the body’s reaction and proper therapy.
Modern methods X-ray contrast studies are not absolutely safe, as they carry a certain risk of complications. However, it is justified, because X-ray research methods are most effective in recognizing urological diseases. Strictly individual approach, the use of a number of possibilities makes it possible to prevent or minimize, and sometimes almost eliminate, the risk during x-ray examinations.
Side effects of radiocontrast agents should be divided into two groups - adverse reactions and complications.
Adverse reactions: headache, dizziness, metallic taste in the mouth, feeling of heat, drop in blood pressure within 20 mm Hg. Art. In most cases, they do not require therapeutic measures and disappear without a trace after the end of the study. However, they can also be harbingers of more serious complications, and therefore they should be treated with attention (monitoring of the patient is necessary).
Complications include allergic manifestations (urticarial and petechial rash, angioedema, lacrimation and salivation, broncho- and laripgospasm), anaphylactic shock, collapse, acute renal and liver failure, death.
Complications require immediate treatment, since if timely assistance is not provided, their severity progressively increases.
When X-ray contrast agents are administered, phenomena of iodism may occur as a result of individual iodine intolerance. In most patients, iodism occurs mildly and is manifested by irritation of the mucous membranes and skin. Cough, runny nose, lacrimation, urticarial rash usually disappear in the first hours, rarely after 1-2 days. Less commonly observed are more severe complications as a result of idiosyncrasy to iodine, which are expressed in laryngo- and bronchospasm, anaphylactic shock.
Often, when a contrast agent is injected, pain is observed along the course of the vessel. Their intensity depends not so much on the properties of the contrast agent, but on its concentration, quantity and rate of administration. When a contrast agent is injected into the cubital vein, the pain is localized along the vein and in the armpit. It is caused by a reflex spasm of the vein and depends on the duration of contact of the contrast agent with the vascular endothelium. More intense pain and a feeling of numbness in the distal part of the arm are observed when a contrast agent is injected into small veins back surface brushes
They are caused by insufficient dilution of the contrast agent in the blood, as a result of which it strongly irritates the intimal receptors, and stretching of a small-caliber vessel with its subsequent spasm. Prolonged spasm of the vein can lead to phlebothrombosis. Sharp pain occurs with paravasal administration of a contrast agent, after which a painful infiltrate appears, which can lead to necrosis of surrounding tissues.
Changes may occur in response to the administration of a contrast agent. physical and chemical properties blood P.V. Sergeev (1971) came to the conclusion that iodine-containing contrast agents reduce the osmotic resistance of erythrocytes, increase hemolysis, cause deformation of erythrocytes and a decrease in ESR as a reflection of the influence of contrast agents on the electrical balance of erythrocytes.
A decrease in the number of red blood cells and hemoglobin content may be observed. W.Vahlensieck et al. (1966) indicate that hemolysis of erythrocytes releases histamine, small doses of which, as a result of the angioneurotic reaction, cause a feeling of heat, a metallic taste in the mouth, spasm of smooth muscle organs and a decrease in blood pressure.
The nephrotoxic effect of radiocontrast agents can be expressed in proteinuria, acute tubular and medullary necrosis and acute renal failure. The underlying pathogenesis of contrast agent nephrotoxicity is vasoconstriction, which can be caused by direct endothelial injury or protein binding, as well as red blood cell agglutination and destruction. These complications may manifest clinically as interstitial tubular nephritis, tubular nephrosis, or shock kidney. Morphologically, vascular disorders are detected: thrombosis, infarction, fibrinoid necrosis of the wall of capillaries, glomeruli, inter- and intralobular arteries.
Signs of acute renal failure may occur in the first hours after the introduction of contrast agents into the blood. Despite renal failure, hypokalemia occurs, then dyspeptic disorders develop, abdominal pain and skin rashes appear, which are usually regarded as a manifestation of intolerance to the drug. Acute renal failure occurs due to ischemia of the renal cortical substance in response to a blood flow disorder.
Morphological data indicate the development of acute interstitial or tubular-interstitial nephritis. Necrosis of the renal cortical substance is occasionally observed. The reason for the nephrotoxicity of some contrast agents may also be a high concentration in the tubular cells of those substances that are normally excreted by the liver, but do not enter the bile due to obstruction of the gallbladder or damage to the liver parenchyma.
In case of liver diseases, especially when its antitoxic function is impaired, when the kidneys compensatoryly provide its neutralizing function, the nephrotoxic effect of contrast agents increases sharply and the occurrence of kidney complications is more likely. Therefore, X-ray contrast studies of the kidneys in hepatopathy are not safe.
There are known cases of acute renal failure after excretory urography in patients with multiple myeloma. In its pathogenesis in patients with multiple myeloma, mechanical blockage of the renal tubules by protein casts occurs, followed by atrophy of the nephrons involved in the process and cessation of urine formation.
During excretory and especially infusion urography, dehydration of the body occurs, so in such patients it is necessary to maximize diuresis and administer a sufficient amount of fluid. This recommendation also applies to patients with proteinuria of unknown origin for whom X-ray contrast examination of the kidneys is indicated.
First aid for adverse reactions and complications caused by intolerance to radiocontrast drugs
At allergic reactions(urticarial and petechial rash, swelling of the tongue, larynx, trachea) first of all, it is necessary to administer intravenously 20-30 ml of a 30% solution of sodium thiosulfate (the best iodine antidote), then 10 ml of a 10% solution of calcium chloride or calcium gluconate, glucocorticoids (100-200 mg hydrocortinosis or 40-60 mg prednisolone in 5% glucose solution), suprastin, diphenhydramine, pipolfen, lasix (20-40 mg).A sudden decrease in blood pressure in combination with a sharp pallor of the skin and a small, weak pulse must be regarded as acute cardiovascular failure and urgent therapeutic measures must be taken.
Acute left ventricular failure(increasing shortness of breath, cyanosis, tachycardia, hypotension, circulatory hypoxia, and in severe cases - pulmonary edema). 0.5-0.7 ml of 0.05% solution of strophanthin or 0.06% solution of corglycon in 20 ml of 40% glucose solution, 10 ml of 10% solution of calcium chloride or calcium gluconate, 2 ml of 2.4% solution of aminophylline are administered intravenously . With the development of pulmonary edema, oxygen, tourniquets on the limbs, intravenous 1.5-2 ml of thalamonal, glucocorticoids (100-150 mg of hydrocortisone or 40-60 mg of prednisolone intravenously in a 5% glucose solution) are used.
Acute right ventricular failure(increasing tachycardia, decreased blood pressure, cyanosis, shortness of breath, a sharp increase in central venous pressure, which in the periphery is manifested by a sharp swelling of the veins and enlargement of the liver). 10 ml of a 10% solution of calcium chloride or calcium gluconate, 10 ml of a 2.4% solution of aminophylline are administered intravenously.
Anaphylactic shock(sudden itching of the skin, a feeling of heaviness, tightness in the chest and epigastric region, shortness of breath, redness of the face gives way to pallor, a drop in blood pressure, sometimes loss of consciousness, convulsions). Intravenous or intracardial injection should be administered 0.5-1 ml of 0.1% solution of adrenaline or norepinephrine, glucocorticoids (100-200 mg of hydrocortisone or 40-60 mg of prednisolone intravenously in 5% glucose solution), ephedrine, diphenhydramine, diprazine. If shock occurs during intravenous administration of a contrast agent into a limb, it is recommended to immediately apply a tourniquet to it [Bunatyan A.A., 1977].
Asthmatic status(or condition); in stage I, an attack of bronchial asthma, but with respiratory failure and moderate hypoxemia and pale cyanosis; in stage II, respiratory failure increases, aggravated by hypoxemia and hypoxia; in III - loss of consciousness and disappearance of reflexes (hypoxic coma). Provide oxygen inhalation. 10 ml of a 2.4% solution of aminophylline and 2 ml of a 2.5% solution of glucose are administered intravenously; intravenous glucocorticoids (200-300 mg of hydrocortisone or 100-150 mg of prednisolone) are administered intravenously to reduce swelling of the bronchial mucosa (20-40 mg).
In case of prolonged status asthmaticus, artificial ventilation is indicated. A.A. Bunatyan et al (1977) do not consider tracheostomy advisable, since it makes sealing difficult respiratory system which is absolutely necessary.
Neurological complications. When epileptiform attacks occur, sodium thiopental is administered intravenously; intubation for anesthesia is performed. In case of damage to the spinal cord (girdling pain, accompanied by contracture of the muscles of the corresponding segment), 10 ml of a 10% solution of calcium chloride and morphine are administered intravenously.
By intravenous administration of a contrast agent using an automatic injector at a rate of 2 to 7 ml per second. For this purpose, as a rule, non-ionic iodine-containing preparations are used at the rate of 2 ml per 1 kg of the subject’s weight. This method allows you to evaluate the structure of blood vessels (CT angiography), identify and evaluate damage to parenchymal organs, etc.
Goals of bolus contrast enhancement
Bolus contrast enhancement is performed to evaluate vessels (CT angiography), to improve differentiation of vessels from lymph nodes, detect and characterize parenchymal organ lesions, evaluate the renal collecting system and urinary tract, identify inflammatory or neoplastic interstitial enhancement, and analyze tissue perfusion.
Radiocontrast agents for bolus contrast
For bolus contrast enhancement, radiopaque agents containing iodine are used, which is due to the presence of relative and absolute contraindications to the procedure, the need preliminary preparation patients from the population at risk of adverse reactions. The use of non-ionic contrast agents can reduce the incidence of adverse reactions; iodinated contrast agents, although moderately well tolerated, are not recommended for use in computed tomography due to the increased risk of complications associated with the high injection rate of bolus contrast.
Technical features
Bolus contrast enhancement is a mechanically guided injection contrast agent using a powerful syringe-injector with set speed administration (in most cases unchanged during the study). This nature of the administration of the contrast agent makes it possible to obtain optimal contrast phases for various purposes.
Contrast phases are directly related to the anatomy and physiology of the circulatory system and blood supply to organs ( see Human circulation). The delay time after the start of administration of the contrast agent before the start of the CT scan is selected taking into account the organ that is the target of the study. Most organs have an arterial blood supply. An exception is the liver and lungs (the liver is supplied with blood not only from the portal vein system - 75-90%, but also from the hepatic artery; the lungs receive venous and arterial blood from the small and big circles blood circulation, respectively). Organs with predominantly arterial perfusion accumulate contrast media best 5-15 seconds after the peak of aortic contrast enhancement. It is preferable to scan the liver in the portal phase, in which contrast enhancement of the organ is noted from both the hepatic artery system and the portal vein system. To improve the quality of diagnosis, scanning in the portal phase with contrast is best preceded by scanning in the arterial phase.
| Department of Cardiovascular System | Time (s) |
|---|---|
| Right atrium | 6-12 |
| Main pulmonary artery | 9-15 |
| Left atrium | 13-20 |
| Aorta | 15-24 |
| Carotid arteries | 16-24 |
| Renal arteries | 18-27 |
| Femoral arteries | 22-33 |
| Jugular veins | 22-30 |
| Renal veins | 22-30 |
| Suprarenal IVC | 24-32 |
| Infrarenal IVC | 120-250 |
| Splenic vein | 30-45 |
| Mesenteric veins | 35-50 |
| Hepatic veins | 50-80 |
| Femoral veins | 120-250 |
Time for the contrast agent to reach parts of the cardiovascular system after injection into the right ulnar vein (according to M. Prokop, A.J. van der Molen)
Complications and adverse reactions
The most common complication with bolus contrast enhancement is extravasation of the contrast agent (its entry into the soft tissue beyond the vascular bed at the injection site). Most often, the volume of extravasation does not exceed 10 ml; large extravasation can cause serious damage to the skin and subcutaneous tissues. Risk factors for the development of extravasation are lack of contact or weakness of patients, multiple punctures of the same vein, injections on the back of the hand and foot. Extravasation is accompanied by local pain and swelling. In case of extravasation of the contrast agent, an elevated position of the limb and cold are prescribed. It is necessary to inform the attending physician about the fact of extravasation and monitor the patient for 2-4 hours. If the volume of ionic contrast agent extravasate is more than 30 ml or non-ionic contrast agent is more than 100 ml, the appearance of blisters on the skin, changes in tissue perfusion or sensitivity in the hands, consultation with a surgeon is advisable.









