Measles vaccination has side effects. Measles vaccination. Is vaccination necessary, when to do it, possible complications, contraindications and types of vaccines.
– an airborne viral infection, children under 5 years of age are most susceptible to this disease. Older children and adults rarely get measles, but they suffer from it more severely than children.
What is the danger of measles
It's better to get vaccinated than to get measlesThe infection poses a mortal danger for children due to complications from the nervous and respiratory systems: slowly progressive pathology nervous system and even disability. The frequency of such severe complications is 1 case per 1000 cases.
80% of sick children develop complications in the form of tracheitis, or, which can subsequently become chronic.
In older children, frequent complications include optic or auditory neuritis.
Mortality from this infection, even with timely and complete treatment in different years reaches 5-10%. The disease poses the greatest danger to children in the first 5 years of life.
What does vaccination give?
From birth to 6-9 months, a child is to some extent protected from measles by maternal antibodies (if the mother has previously had measles or has been vaccinated against it). But even infants can get sick if the titer of maternal antibodies is low or the virus is highly aggressive.
Importance of measles vaccination:
- Protects against infections that are dangerous for children and the complications it leads to;
- prevents the occurrence of epidemics;
- limits the circulation of the pathogen in the population;
- the vaccine attenuated virus reduces the load on the immune system (compared to fighting the wild virus) during formation.
Vaccines used
The following vaccines can be used for vaccinations:
- monovalent - live dry measles vaccine (Russia) and "Ruvax" - (France);
- polyvalent vaccines (with several components): measles and (Russia); against measles, rubella, mumps (Priorix Belgium, Ervevax UK, MMR II USA);
 Measles vaccine
Measles vaccine The effectiveness of all vaccines is the same, any of them can be used, they are all safe. Moreover, they are interchangeable: if one drug was used first, then another can be administered: negative consequences it won’t and it won’t affect the efficiency.
If a child has previously had one of the infections, then you can choose a drug without this component, or you can vaccinate with a vaccine containing a component of the previous disease: this will not cause harm, the component will be destroyed by specific antibodies. This will not affect the formation of immunity against other infections.
The live viruses in the vaccine are weakened and are not dangerous for the child or unvaccinated children around him.
Vaccination calendar
According to the calendar, measles immunization is carried out for children of the following age categories:
- at 1 year;
- at 6 years of age;
- from 15 to 17 years of age.
The first injection of the vaccine can be carried out at 9 months. in the event that the mother has never been vaccinated against measles and has not had it (that is, the baby has not received protective antibodies from the mother). Subsequent injections of the vaccine are carried out from 15 to 18 months, at 6 years and from 15 to 17 years.
 If the child has not been vaccinated, he is vaccinated according to an individual scheme
If the child has not been vaccinated, he is vaccinated according to an individual scheme If a child under 6 years of age has not received measles vaccinations for any reason, then the vaccine is administered at the first opportunity, and the second dose is administered at 6 years of age (but not earlier than six months from the first vaccination); The third vaccination is given at 15-17 years of age.
If a child over 6 years of age has not been vaccinated against measles, then, if possible, the vaccine is administered twice with an interval of 6 months, and according to the calendar - at 15-17 years of age.
The measles vaccine is administered intramuscularly or subcutaneously. The optimal sites for insertion are the outer surface of the shoulder, subscapularis, or thigh.
The effectiveness of immunization when vaccinated at 9 months. – 85-90%, at one year of age – reaches 96%. Immunity is formed from the 2nd week after vaccination. The second dose of the drug is administered with the goal of providing 100% coverage of children with reliable protection against measles before starting school. The third dose is administered to maintain immunity for more long period.
Reaction to vaccination
The reactogenicity of the measles vaccine is very low, and there are practically no complications after vaccination. Live, but significantly weakened viruses in the drug cannot cause full-blown measles disease. During the day after the injection, there may be a slight increase in temperature, a slight thickening and mild pain at the injection site.
 The reaction to the vaccine may be local
The reaction to the vaccine may be local Depending on the individual reaction of the body, the temperature rise can reach high numbers. Fever lasts up to 4 days. Since it does not affect the formation of immunity, the child can be given antipyretics (Ibuprofen, Paracetamol) to avoid the development of febrile seizures.
Sometimes (5%-15%) a post-vaccination reaction may manifest as skin rashes.
Delayed reactions to the vaccine may occur 5-15 days after injection. In this case, the symptoms resemble measles, and many parents consider the reaction to be vaccine-related measles. However, the phenomena soon disappear on their own. More often, a delayed reaction occurs after the first dose of the vaccine.
If morbilliform symptoms appear more than late period(more than 2 weeks after vaccination), then they should be regarded as measles due to unformed immunity.
Summary for parents
 Prevention is better than cure
Prevention is better than cure Parents who consider measles to be a minor childhood disease that is best dealt with during childhood should reconsider their opinion. The argument for this is the frequency of severe complications of measles, especially in young children.
Reliable protection against the disease is vaccination, which can be combined with vaccinations against other infections using polyvalent vaccines.
Parents who are afraid of complications after vaccination should know the statistics: encephalitis after vaccination develops with a frequency of 1 case per 100,000 vaccinated people and 1 case per 1000 cases of measles. That is, the risk of a serious complication after vaccination is 100 times less likely than in the case of a child who fully develops measles.
Which doctor should I contact?
Before vaccination, the child must be examined by a pediatrician. He also develops an individual vaccination schedule. If necessary, parents can consult an infectious disease specialist, allergist, or immunologist.
Each of us knows that it is much easier to prevent a disease than to treat it later. The same can be said about measles. Universal vaccination has reduced the number of cases of this disease by 90%. Which once again proves the effectiveness of vaccination.
Danger of measles
Measles is a dangerous viral infection transmitted by airborne droplets, to which unvaccinated children are more susceptible. Among adults and adolescents, this disease is diagnosed much less frequently.
The source of infection is usually a sick person. The incubation period for measles is 7-17 days. In a normal environment, the virus dies quickly enough, so to protect others it is enough to simply ventilate the room in which the patient was.
Measles can lead to the following complications:
- pneumonia;
- encephalitis - inflammation of the brain;
- Thrombocytopenia is a significant decrease in the number of platelets in a person’s blood. In case of illness, their number decreases to 150*109/l or less, with the norm being 180-320*109/l;
- ear infections.
To date, measles vaccination is the only in an effective way preventing infection with a dangerous virus. Since small children who come into contact with other children are most susceptible to it, measles vaccination has been included in the mandatory vaccination schedule.
- women of childbearing age;
- medical and educational institutions where there is a risk of infection;
- for those planning to visit countries where measles cases have been reported.
If a person has been in contact with a person with measles, he is recommended to undergo unscheduled vaccination within 3-7 days from the date of contact.
Find out Dr. Komarovsky's opinion regarding measles vaccination in the video:
Contraindications
Despite the importance of vaccination, measles vaccinations are contraindicated in the following cases:
- allergic reactions to other vaccines and medications;
- the presence of HIV infection in the human body;
- cancer;
- woman's pregnancy;
- tuberculosis disease;
- taking blood products;
- during the acute period of any disease;
- if there are disturbances in the immune system, which is observed after organ transplantation;
- if there is an insufficient number of platelets in the patient’s blood.
Vaccination for children
![]() The vaccination schedule depends on whether it is a planned vaccination or an emergency one.
The vaccination schedule depends on whether it is a planned vaccination or an emergency one.
Scheduled vaccination according to the vaccination calendar is carried out for the first time every 1-1.5 years of the baby. The second vaccination is given at 6 years of age. The minimum permissible interval between vaccinations cannot be less than 4 years. Modern vaccines work well together. Therefore, the vaccine against measles is often given together with vaccinations against rubella and.
The measles vaccine is quite reliable and protects the child for a long period. A repeat dose, which is administered during revaccination, is necessary to ensure that the child receives lasting immunity for life.
But there are situations when a deviation from the vaccination schedule is required:
- When a case of measles is diagnosed, the vaccine is given to everyone who was in direct contact with the patient. This category includes everyone aged 1 to 40 years who has not had this disease and has not received vaccinations according to the calendar.
- If a woman gives birth to a child whose body does not have antibodies to the disease, it is recommended to vaccinate him at the age of 8 months. This will make it possible to reduce the likelihood of infection of the baby. He will be vaccinated a second time at the age of 15 months and beyond according to the calendar.
- At the age of six months, children who live in regions with a difficult epidemiological situation are vaccinated against measles.
The vaccine should be administered under the skin in the forearm area (for children) or under the shoulder blade (for adults).
It can only be done in vaccination clinics. There you are required to provide all the information regarding the drug. If a patient suffers from any type of allergy, before administering the vaccine it is necessary to conduct a special test under the supervision of an allergist.
Those who have already had measles do not need to be vaccinated, since after recovery a person develops stable, lifelong immunity and is no longer afraid of the virus.
Side effects
To vaccinate children against measles, a live vaccine with a weakened virus is used. Therefore, approximately 10% of vaccinated children may develop vaccine measles, a mild form of the disease. Its symptoms include fever and a small skin rash, which are not at all dangerous to others and are easier to tolerate than ordinary measles.
In extremely rare cases, vaccinated children are diagnosed with measles. However, this percentage is too small and is comparable to the number of cases in which a child was infected with the virus twice.
Simply put, without vaccination, the risk of the disease is 100%, while a person who has been vaccinated or has already had measles can only get sick in 0.5% of cases. At the same time, re-infection and infection of vaccinated children always occurs in a mild form. 
Features of adult vaccination
Despite the fact that measles has always been considered a childhood disease, adults can also encounter it. Moreover, in mature age The disease is much more difficult to tolerate and can cause complications. People whose bodies lack vitamin A are primarily susceptible to the disease. Therefore, all adults who do not monitor their diet are at risk.
In order not to expose yourself to danger, it is recommended that all adults who have not had this infection and were not vaccinated in childhood be vaccinated against measles. This especially applies to those who come into contact with a large number of people and have weakened immune systems.
The administration of the drug is tolerated quite easily by adults, and the vaccination itself can protect against the disease for 19 years.
Vaccination and pregnancy
Any virus is very dangerous for pregnant women and developing fetus. In case of illness on early stages pregnancy, women experience miscarriage. If the pregnancy was maintained, then almost half of the children begin to develop various pathologies. Modern polyvalent vaccines contain minimum quantity virus, therefore they are considered gentle on the fetus. If a woman does get measles during pregnancy, she is given an injection of immunoglobulin.
To avoid infection during pregnancy, doctors recommend that a woman be vaccinated at the stage of planning pregnancy. After giving birth, a woman will be able to get vaccinated no earlier than 2-3 weeks later.
Possible consequences
 Often, the measles vaccine does not cause adverse reactions. In isolated cases, body temperature may rise and skin rashes may appear. All adverse reactions go away on their own within a few days.
Often, the measles vaccine does not cause adverse reactions. In isolated cases, body temperature may rise and skin rashes may appear. All adverse reactions go away on their own within a few days.
Children with allergies are susceptible to urticaria, angioedema, or even anaphylactic shock after administration of the drug. An increase in temperature in such children can lead to seizures. To prevent such reactions, pediatricians recommend giving the child paracetamol on the 5th day after the vaccine is administered.
In extremely rare cases, when the vaccine is initially administered to children who have not previously had measles, encephalitis and thrombocytopenia may develop.
In any case, it should be remembered that vaccination extremely rarely leads to complications, but it can save health and life in the event of infection with a dangerous virus.
Measles vaccines
There are monovaccines and polyvaccines, which contain components that protect not only against the measles virus. The monovaccine is usually used to vaccinate adults.
Children are recommended to be vaccinated with a divaccine (measles and mumps) or a trivaccine (measles-rubella-mumps). In terms of tolerability, they are all identical and are capable of protecting a person from infections for a long period.
Experts' opinion about measles and vaccination against this disease in the video:
Is it possible to get sick after vaccination?
There is a chance of contracting the measles virus after vaccination, but it is minimal. Most often, people who get measles get only one instead of two recommended vaccinations. After all, it is after revaccination that stable immunity is formed in the human body.
There is also a possibility of infection for a person who was vaccinated more than 10 years ago and was not revaccinated. This is due to the fact that over time (usually 10-20 years) the protection decreases, which can cause the virus to develop in the human body.
When faced with a choice whether to vaccinate their child against measles or not, parents should always remember that it is the only possibility prevent your baby from getting a dangerous infection. In case of infection, the vaccine can reduce the possibility of developing complications to zero.
Which annually claims hundreds of thousands of lives around the world. Only the measles vaccination can help protect against this serious disease. Let’s take a closer look at how long vaccination lasts, how long the body’s resistance to measles lasts, and what this disease actually is.
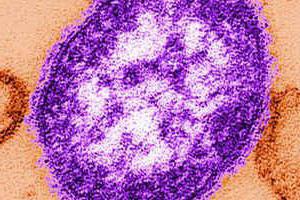
Measles
An RNA virus is considered the causative agent of the disease. In general, measles is more of a childhood disease, but if an unvaccinated adult becomes infected with the virus, the course of the disease for him is most severe. complex form, leaving behind various complications. The virus spreads when the patient coughs, sneezes with particles of mucus, or when talking with saliva. An infected person becomes contagious even when he himself does not feel symptoms of the disease, that is, during the incubation period. The only protection is the measles vaccination. How long it acts in the body is a question that interests many. You are guaranteed to be protected for 10-12 years, as doctors say.
If the virus has entered an unprotected body, the patient begins to notice symptoms that are more typical of many respiratory diseases:
- fever (temperature up to 40 degrees);
- sore throat, sore throat;
- dry cough, runny nose;
- weakness, malaise;
- headaches.
Specific signs of measles include the following symptoms:
- conjunctivitis and photophobia;
- severe swelling of the eyelids;
- rashes on the mucous membranes of the cheeks appear on the second day (whitish small spots like grains of semolina, which disappear after a day);
- on the 4-5th day - a rash on the skin, first it appears on the face, then spreads down throughout the body.

Possible complications of measles
Vaccination against measles will save you from the disease. As long as it works, the body will be protected from infection. In unvaccinated children, and even more often in adults, measles causes serious complications:
- measles or bacterial infection often causes pneumonia;
- bronchitis;
- sinusitis;
- keratitis (every 5th patient loses vision);
- meningitis and meningoencephalitis;
- otitis and eustachitis (later - hearing loss);
- pyelonephritis.
There is no effective antiviral treatment for measles. Only vaccination carried out in advance can save a person! In 0.6% of cases, measles is complicated by brain damage (encephalitis), and 25% of patients die.
When to vaccinate
In Russia, vaccination against measles has been introduced into the scheduled vaccination calendar. A child is vaccinated at the age of 1-1.3 years. Revaccination is carried out at 6 years of age.
Due to the fact that the increase in the disease in 2014 in Russia led to serious consequences among the adult population, it was decided to vaccinate the population. According to the national program, free measles vaccination is introduced up to the age of 35. How long does the drug last? On average, the immunity of a vaccinated person is resistant to the disease for up to 12 years (sometimes longer).
What should people over 35 do? Vaccination is carried out to everyone, but on a paid basis. The monovaccine is administered twice with a three-month interval. If you once received one vaccine, you need to get vaccinated again. Revaccination is not carried out for adults.
Emergency immunization
Regardless of the vaccination calendar and schedule, emergency immunization is carried out in the following cases:
- In the source of infection, all persons in contact with the patient are vaccinated within three days (free of charge). Unvaccinated children over one year of age are included.
- For a newborn, if anti-measles antibodies are not detected in the mother’s blood. The baby is re-vaccinated at eight months, and then according to the calendar.
- When traveling abroad, a measles vaccination must be done one month before departure. Special attention those traveling to Georgia, Thailand, Ukraine, where over the past 3 years many cases of measles with a fatal outcome have been recorded. Field services know how long the measles vaccination lasts. Vaccination will be noted in your documents, and this will allow you to travel abroad without fear for many years.
- Unvaccinated women who are planning a pregnancy, since during pregnancy, measles is very dangerous for the fetus.
- Persons from 15 to 35 years old who do not have proof of vaccination and if they are in risk groups (teachers, health workers, students).

Where is the vaccine given?
When administering the measles vaccine, you must follow some rules that every physician must know about, as well as how long the measles vaccine lasts.
For children, the drug in an amount of 0.5 ml is injected into the subscapular region or just below the middle third of the outer surface of the shoulder.
For adults, the vaccine is injected into the muscle or subcutaneously into the upper third of the shoulder. The drug is not recommended to be administered into the gluteal region due to an excess of subcutaneous fat. Intradermal contact is also undesirable. Injection into a vein is strictly contraindicated!
Vaccination of both children and adults should always be carried out with written consent. If there is a refusal to vaccinate, it must also be made in writing. The waiver must be renewed annually.
How long does the measles vaccine last?
So, for how long after a measles vaccination is our immunity strong against this terrible disease? If we talk about adults, the average validity period lasts 12-13 years. There are cases where a period of 10 years is indicated. If we delve into this issue more deeply, it is worth saying that everything is individual. “Post-vaccination immunity” (there is such a concept) can be different for each individual, for some it will be 10 years, for others 13 or even more. There was a recorded case where a patient showed antibodies to measles already 25 years after vaccination.
It is also important to understand that if you are vaccinated, this will not provide a 100% guarantee of protection. As the vaccine developers themselves claim, you simply have a much better chance of not getting sick than those who are not vaccinated.
How long does it take for the measles vaccine to take effect? This happens as soon as your body forms immunity (antibodies) to the disease. On average, this occurs after 2-4 weeks after vaccination. Each case is individual.
![]()
Measles vaccination contraindications
We have found out how long the measles vaccine lasts in adults; now we will figure out what contraindications to the vaccine exist. The most serious ones include the following:
- It is not recommended to administer the vaccine to pregnant women. If there is a need, it is necessary to consult with specialists.
- Vaccination is contraindicated for patients with AIDS, HIV, as well as those who have diseases affecting the bone marrow or lymphatic system.
- You should not get vaccinated if you at the moment you have an aggravation of any of your chronic diseases.
- If you have general ailments or diseases, also postpone vaccination.
- Vaccination is also contraindicated if it has previously caused complications for you.
- Be sure to check with your doctor to see if the medications you are taking are compatible with this vaccine.
- Allergy to egg white.
- Malignant neoplasms.
- Antibiotic intolerance.
Common effects of measles vaccination in adults
Adults begin to feel the effects of vaccination on the first day. There may be pain at the injection site, redness of the skin, and some thickening. Similar symptoms are common with other types of vaccination, for example, against hepatitis B.
Further, depending on your immunity, often on the fifth, and for some on the tenth day, lethargy, fatigue, and body temperature rise. This is considered normal because your body begins to produce antibodies to measles. You need to inform your doctor about your condition, he will competently explain the cause of the ailment and fill you in on how long the measles vaccine is valid. These are the main consequences of the measles vaccine that all normal, healthy people experience.

Side effects of vaccination
In rare cases, adverse reactions to the vaccine occur, some of which can be considered severe. You can’t do this without the help of doctors. They may be as follows:
- A toxic reaction can occur 6-11 days after vaccination. The temperature rises, a sore throat occurs, intoxication occurs, and a rash appears. The period may last five days, but it should be distinguished from any infectious diseases.
- Convulsive or encephalic reaction. High temperature and seizures. Most pediatricians do not classify these symptoms as severe complications.
- Post-vaccination encephalitis. Symptoms resemble those of other infections: dizziness, headaches, nausea, confusion, agitation, convulsions, neurological symptoms.
- Allergic reactions to vaccine components. Quincke's edema. Hives. Joint pain.
- Exacerbation of allergic diseases. Bronchial asthma.
- Anaphylactic shock.
- Pneumonia.
- Myocarditis.
- Meningitis.
After all of the above, many may have the impression that vaccination is dangerous. But that's not true. Many side reactions are formulated purely theoretically. For example, a complication in the form of encephalitis can occur once in a million. If measles occurs, the risk of complications increases thousands of times.
How long does it take for the measles vaccine to take effect? As soon as antibodies are formed in the body (from 2 to 4 weeks). If during this time you do not feel any side effects in the body, a trip to the doctor is not necessary.
Treatment of complications after vaccination
How long does the measles vaccine last? For a long time (from 10 to 13 years) you will be protected from the disease. It is worth considering that the body’s reactions, even if they occur, pass quickly, after a few days, but complications after the disease itself can be disastrous, even fatal.
- If negative reactions occur, consult your doctor.
- Symptomatic medications will help to cope with the consequences: antiallergic, antipyretic.
- If the complication is severe, it is better to treat it in a hospital. The doctor will prescribe you corticosteroid hormones.
- If bacterial complications arise, antibiotics will help to cope with them.

Types of vaccines
Measles vaccine is made from live but very weakened measles viruses. In medicine, both single vaccines (for measles) and combined ones (for measles, mumps and rubella) are used. The vaccine virus itself is not capable of causing the disease in the body; it only promotes the production of measles-specific antibodies. Features of the live vaccine:
- To prevent the drug from losing its potency, it should be stored at a temperature no higher than +4 degrees.
- Unused vaccine is destroyed according to special rules.
- The composition includes egg white and antibiotics. This may cause allergic reactions in some people.
In Russian clinics, domestically produced drugs are used for vaccination - mumps-measles vaccine and measles monovaccine. Single vaccines have fewer adverse reactions.
We found out how long it takes for the measles vaccine to work, what side effects and contraindications there may be. Well, now let’s talk about how to prepare for vaccination so that vaccination is as successful as possible.
What's the best way to get vaccinated?
- You need to come for vaccination absolutely healthy, without any signs or manifestations of ARVI.
- Before vaccination, ideally you will visit a doctor and undergo all general tests.
- After the vaccine is administered, avoid visiting crowded places for three days to avoid contracting any foreign virus.
- Is it possible to swim? Yes, but do not rub the injection site. It's better to take a shower rather than a bath.
- After vaccination, you should not introduce any new foods or dishes into your diet, so as not to provoke allergic reactions.
How long does the measles vaccine last? For more than ten years in your life you can be calm. A terrible disease is unlikely to affect the body, because thanks to vaccination you have developed a strong immunity to measles.
Many infections are much more dangerous for adults than for children. One such disease is measles, which kills 165,000 people worldwide every year. Recent years The incidence of measles in adults in Russia has become more frequent due to a decrease in immunity against this disease. People born after 1956 have lost their immunity, which was acquired as a result of vaccination at 1 year of age or after an illness. Measles vaccinations were mandatory for children in Russia in 1980. In 2014, Russia introduced routine measles vaccination for all adults. Vaccinations are carried out with a vaccine (live measles culture vaccine).
At what age can adults be vaccinated against measles? Should I get this vaccine or not? - let's look at these questions.
What kind of disease is measles?
It is considered a childhood infection, but adults also become infected with it. The causative agent of the disease is an RNA virus from the Morbillivirus family. Infection occurs from another patient. The virus is transmitted through contact by sneezing, coughing, or runny nose. The incubation period is 1–2 weeks. The disease becomes contagious within the last 2 days incubation period when there are no signs of the disease yet. The disease begins with general symptoms:
- runny nose, cough, sore throat;
- temperature rise to 39–40 °C;
- conjunctivitis, accompanied by photophobia and lacrimation;
- swelling of the cheeks and face;
- spots localized on the mucous membrane of the cheeks near the molars and on the gums appear on the 3rd day;
- rash all over the body.

Filatov-Kolsky spots on the oral mucosa are an important sign for diagnosis. Skin rashes differ in the order of appearance and disappearance. It appears on the 3rd day from the day the temperature rises, first on the face, neck, chest, then moves to the torso and limbs. The rashes last for 3 days and begin to fade and disappear in the same order in which they appeared. There is no specific treatment for measles.
Why is measles dangerous for adults?
Measles in adults significantly reduces immunity. The disease is much more severe than in children. The following complications often occur:
- pneumonia caused by measles virus or bacterial infection;
- bronchitis;
- otitis;
- hepatitis;
- eye damage in the form of keratitis leads to loss of vision in 20% of cases;
- pyelonephritis;
- Eustachitis is severe and can lead to hearing loss or hearing loss;
- meningitis;
- meningoencephalitis.
Dangerous complications of measles in adults:
Meningoencephalitis is a virus affecting the human nervous system. The complication occurs in 0.6% of cases. After the temperature drops at the end of the rash, the temperature suddenly rises sharply again, consciousness becomes confused, and convulsions appear. There is no specific treatment. Measles encephalitis is the cause of death in 25% of cases.
The only effective way to protect yourself from a dangerous infection is to vaccinate children and adults against measles.
When to vaccinate
 As part of the national program, routine measles vaccination for adults is regulated by a schedule. There is a specific vaccination schedule throughout the country that determines when and how many times adults should be vaccinated against measles. Free vaccination is provided to people under 35 years of age who have not been sick before and have not been vaccinated or who do not have information about their vaccinations. Those persons who have had contact with measles patients, regardless of age, are vaccinated without payment, if they have not been vaccinated before and have not had this disease. For other persons, paid vaccination is carried out.
As part of the national program, routine measles vaccination for adults is regulated by a schedule. There is a specific vaccination schedule throughout the country that determines when and how many times adults should be vaccinated against measles. Free vaccination is provided to people under 35 years of age who have not been sick before and have not been vaccinated or who do not have information about their vaccinations. Those persons who have had contact with measles patients, regardless of age, are vaccinated without payment, if they have not been vaccinated before and have not had this disease. For other persons, paid vaccination is carried out.
Adults receive 2 vaccinations with a 3-month interval between them. If an adult has been vaccinated against measles once, then he is vaccinated from the very beginning, according to a 2-fold schedule.
There is no revaccination against measles in adults. Immunity after a double vaccination lasts for at least 12 years or more.
Where do adults get the measles vaccine? It is done in the upper third of the shoulder subcutaneously or intramuscularly. It is not recommended to vaccinate in the gluteal region due to the abundant subcutaneous fat layer. The vaccine is not given into the skin, where a lump may form. In both cases, vaccination rules are violated. Intravenous administration of the vaccine is contraindicated.
 According to WHO, in 2013 the epidemiological situation with measles worsened in 36 EU countries, where 26,000 cases of infection were recorded. Most cases of the disease are observed in Germany, Turkey, and Italy. Currently, fatal measles infections have been reported in Georgia and Ukraine. In Russia, cases of imported measles infection from countries visited by Russian tourists have become more frequent: China, Singapore, Italy, Turkey.
According to WHO, in 2013 the epidemiological situation with measles worsened in 36 EU countries, where 26,000 cases of infection were recorded. Most cases of the disease are observed in Germany, Turkey, and Italy. Currently, fatal measles infections have been reported in Georgia and Ukraine. In Russia, cases of imported measles infection from countries visited by Russian tourists have become more frequent: China, Singapore, Italy, Turkey.
When planning a trip abroad, find out when adults are vaccinated against measles. Vaccination against measles is done according to the planned calendar, but you can get an emergency vaccination at any time a month before your expected departure.
What vaccines are used
- “Live cultural measles vaccine” is produced in Russia and registered in 2007. The virus for it is grown in Japanese cell culture quail eggs.
- , manufactured by Merck Sharp&Dohme (Holland). Live vaccine, measles, mumps, rubella.
- Belgian production company GlaxoSmithKline Biologicals. Live measles, mumps, rubella vaccine.
Which vaccine to choose - domestic or imported?
 The Priorix and MMR II vaccines are complex; they produce immunity against 3 diseases at once: measles, rubella, and mumps. Priorix can be used for vaccination not only against three infections simultaneously, but also separately for each disease.
The Priorix and MMR II vaccines are complex; they produce immunity against 3 diseases at once: measles, rubella, and mumps. Priorix can be used for vaccination not only against three infections simultaneously, but also separately for each disease.
The Russian vaccine produces antibodies only against measles.
All drugs have typed viruses and form stable immunity. Complex vaccines are interchangeable. Vaccination can be done with one vaccine, and revaccination with another.
According to the National Vaccination Calendar, Russian vaccines are supplied to clinics. Imported vaccines are purchased at your own expense.
The virus for the live measles culture vaccine is grown in cell culture of Japanese quail eggs.
Live measles cultural vaccine is given in a dosage of 0.5 milliliters twice with an interval of 3 months. Immunity is provided for a period of about 20 years.
The MMR II and Priorix vaccines in adults are given a single dose of 0.5 ml at any age and repeated every 10 years.
Indications for vaccination for adults
The vaccine is given:
- for routine vaccination of all adults simultaneously against rubella, measles and mumps;
- for emergency prevention when planning travel;
- emergency prevention is done in case of contact with a person with measles; the vaccine in such cases is administered within 3 days after contact.
Vaccination when planning a trip abroad should be carried out 1 month before the planned trip.
Vaccination contraindications for adults
Measles vaccination for adults has contraindications. Temporary contraindications are respiratory infection or exacerbation of existing diseases. In this case, the vaccination is delayed for a month.
 Absolute contraindications:
Absolute contraindications:
- allergic reaction to chicken and quail eggs;
- allergy to antibiotics;
- allergic reaction to a previous vaccination;
- pregnancy and lactation period.
What reactions can there be to the vaccine?
Typically, adults have a mild reaction to the measles vaccine:
- redness at the injection site;
- elevated temperature no more than 37.5 °C;
- runny nose, cough;
- joint pain.
 The measles vaccine sometimes causes dangerous side effects in adults:
The measles vaccine sometimes causes dangerous side effects in adults:
- allergic shock;
- hives;
- possibly the appearance of allergic Quincke's edema.
After vaccination against measles, adults rarely experience severe consequences:
- encephalitis;
- myocarditis;
- meningitis;
- myocarditis;
- pneumonia.
To avoid a severe reaction to a vaccine, adults must be healthy on the day of vaccination. Before vaccination, you should consult your doctor and inform him of any allergies to antibiotics or chicken protein and not eat unfamiliar foods.
Due to the deterioration of the epidemiological situation in Russia and in all countries of the world, there is an urgent need to routinely vaccinate all adults against measles. Vaccinations are carried out according to the schedule of the National calendar with Russian and imported vaccines. All vaccinations are safe, interchangeable and effective. In order to minimize the occurrence of complications, you need to prepare for vaccination.
Measles is a fairly serious infection that, before administration, vaccinations As a measure to prevent the disease, 90% of children under the age of 10 were ill. Measles is contagious, transmitted through airborne droplets or direct contact. Moreover, the one that causes infection circulates exclusively in the human population. In contrast to the popular belief that for children, measles is a harmless infection that is best dealt with by the child, the mortality statistics for this disease do not look so rosy.
As of today, the mortality rate from measles, even with timely and high-quality treatment, ranges from 5 to 10%. In 2001, on the recommendation of the World Health Organization, vaccinations measles were introduced into the national calendars or immunization programs of many countries, as a result of which by 2008 it was possible to reduce the number of deaths from the infection from 750,000 to 197,000, that is, almost 4 times.
In addition to being fatal, measles can present with adverse consequences such as encephalitis, protein-losing enteropathy, sclerosing panencephalopathy, and slowly progressive pathology of the nervous system. The incidence of these serious complications ranges from 1 case in 1000 cases to 1 in 10,000.
Measles vaccination
To date, measles vaccination has shown high effectiveness in preventing cases of the disease, as well as a significant reduction in the number of deaths as a result of the unfavorable course of the disease. Immunization against measles is necessary for all people, especially children under 5 years of age, since it is in this age group that the infection is most severe and the risk of death or complications is higher than in older children.It is known that the course of measles is aggravated by the lack of A in the body, caused by a defective adult or child. Therefore, if the child’s living conditions are far from ideal, and the quality of nutrition does not meet the standards for the consumption of vitamins and minerals, it is necessary to get vaccinated to prevent infection.
Currently, there are monovalent measles vaccines, which contain only one component, and polyvalent ones. Polyvalent ones contain several components (not only against measles). Today the following polyvalent vaccines with an anti-measles component are produced in the world:
1.
Measles, rubella.
2.
Measles, rubella, mumps.
3.
Measles, rubella, mumps, chicken pox.
The effectiveness of monovalent vaccines against measles and polyvalent ones with a measles component is the same, so the choice of drug is determined by factors of convenience, etc. The World Health Organization allows only effective and safe measles vaccinations to enter the pharmaceutical market, so any vaccine can be used. In addition, all measles vaccines have the property of being interchangeable, that is, one vaccination can be carried out with one drug, and the second with a completely different one, this will not affect the effectiveness in any way and will not cause any negative consequences.
The measles vaccine is produced in the form of a specially dried powder - lyophilisate, which is diluted with a solvent before administration. The drug should be stored cold or frozen, at a temperature of –20 to –70 o C, but the solvent should not be frozen.
When using the vaccine, it should be remembered that after diluting the lyophilisate, the finished product, left for 1 hour at a temperature of 20 o C, will lose exactly half its ability to fight infection. And when the drug, ready for administration, is left for 1 hour at a temperature of 37 o C, it completely loses its properties and actually becomes unsuitable for use. In addition, the measles vaccine loses its properties when exposed to direct sunlight, so it must be stored in painted bottles. After dissolving the vaccine preparation, it should be stored in the refrigerator for no more than 6 hours. After this time, all unused vaccine should be discarded.
Measles-rubella-mumps vaccination
The measles-rubella-mumps vaccine contains three components that allow you to administer a drug in one injection that initiates the formation of immunity to not one, but three infections at once. This vaccine has low reactogenicity, which is no higher than a monovalent vaccine exclusively against measles.In the measles-mumps-rubella vaccination, various subtypes of the measles virus can be used, for example, Edmonston, Enders, Peebles, Schwartz, Edmonston-Zagreb, Moraten and AIC - C, CAM - 70, TD - 97, Leningrad - 16, Shanghai - 191. The differences between all these types of vaccine viruses are insignificant and do not exceed 0.6%. At the same time, the maximum variability is observed in strains SAM - 70, TD - 97, Leningrad - 16, Shanghai - 191. Any type of vaccine type of measles creates excellent immunity against the wild measles virus. To date, no variants of transmission of the vaccine type of measles virus from a vaccinated person to another have been identified.
The complex three-component measles-rubella-mumps vaccine contains sorbitol, hydrolyzed gelatin and the antibiotic Neomycin as preservatives and stabilizing substances. Thanks to these stabilizer substances, the measles-rubella-mumps vaccine does not contain the mercury compound thiomersal (merthiolate) as a preservative. Thanks to this, the danger of possible side effects from the ingestion of mercury compounds into the body is completely eliminated, which makes the drug completely safe.
However, the absence of a preservative, merthiolate, imposes strict storage conditions for the vaccine. Until dissolved, the lyophilisate is stored cold or frozen, at a temperature not lower than –70 o C. Before administering the vaccine, the powder is diluted; this solution must be placed in a painted bottle, since the drug is not stable when exposed to sunlight. The prepared solution can only be used within 6 hours, provided it is stored in the refrigerator during this period of time. If the solution stands for 1 hour at a temperature of 20 o C, then it will lose half its properties, and the same period of time at 37 o C - the vaccine will become completely spoiled.
The measles-rubella-mumps vaccine is convenient for vaccination because it reduces the number of injections and trips to the clinic. If a child or adult has already had an infection (for example, measles, rubella or mumps), then you can choose a vaccine without a component that the human body has already encountered. But you can also get the measles-rubella-mumps vaccine - then the component that the person has already had will be simply destroyed by the existing immune cells. In this case, the vaccine will not cause harm, but will only help to develop immunity to other infections, the components against which the complex drug contains.
Do you need a measles vaccination?
 The measles vaccine has the following: positive properties– prevents epidemics of infection, reduces mortality and disability, and also allows limiting the circulation of the virus in the population. The reactogenicity of the measles vaccine is very low, and there are practically no complications. For example, a complication such as encephalitis occurs in 1 case out of a thousand sick people, and in 1 case out of 100,000 vaccinated people. As you can see, the risk of developing a serious complication in the case of measles vaccination is 100 times less than in the case of a complete infection.
The measles vaccine has the following: positive properties– prevents epidemics of infection, reduces mortality and disability, and also allows limiting the circulation of the virus in the population. The reactogenicity of the measles vaccine is very low, and there are practically no complications. For example, a complication such as encephalitis occurs in 1 case out of a thousand sick people, and in 1 case out of 100,000 vaccinated people. As you can see, the risk of developing a serious complication in the case of measles vaccination is 100 times less than in the case of a complete infection. There is an opinion that it is better to get infections such as measles, rubella or chickenpox in childhood, since they are better tolerated and then provide immunity for life. However, this position is very one-sided and irresponsible. Thus, vaccination ensures a significant reduction in the number of circulating viruses in the population, since vaccinated people do not get sick, and the microbe simply has nowhere to live and reproduce. In this case, with an active immunization policy, it is possible to eliminate the measles virus from the human population - then the next generations can easily do without vaccination, as, for example, happened with smallpox, for which they have not been vaccinated since the 80s of the 20th century. Therefore, immunizing children against measles may help grandchildren who may not need it at all. Otherwise, each generation of children will be forced to suffer from measles and other infections, continuing this vicious circle.
Newborn babies are protected from measles for some time, so they are rarely infected. If the mother had measles or was vaccinated against the infection, then the antibodies in the child’s blood remain for 6 to 9 months, providing him with immunity from the disease. However, this is not a guarantee, since if the antibody titer is low or the virus is highly active, the child can still get this dangerous infection.
Measles is not at all as harmless as is commonly believed, since in 80% of cases this infection is complicated:
- average ;
- laryngitis;
- pneumonia.
Due to all of the above factors, there is an objective opinion that a child still needs a measles vaccination. It will help protect him from the risk of chronic post-measles inflammatory diseases of the respiratory system, and will reduce the load on the immune system without forcing it to fight a full-fledged pathogen.
Why measles vaccination is necessary - video
Measles vaccination for adults
 Today in Russia the need for measles vaccination in adults is due to two main reasons. Firstly, the country has an unfavorable epidemiological situation, there is large number migrants from other regions who are carriers of various infections, including measles. Therefore, in order to activate the immunity against measles acquired in childhood, adults under 35 years of age are given another dose of the vaccine.
Today in Russia the need for measles vaccination in adults is due to two main reasons. Firstly, the country has an unfavorable epidemiological situation, there is large number migrants from other regions who are carriers of various infections, including measles. Therefore, in order to activate the immunity against measles acquired in childhood, adults under 35 years of age are given another dose of the vaccine. Secondly, in a number of regions of Russia, thanks to the efforts made to vaccinate children against measles, it was possible to reduce the number of cases of the disease by 10-15 times. Typically, the vaccine works effectively for 20 years, after which revaccination is necessary. However, when the incidence of measles was higher, the number of circulating viruses was greater, then the immune system of vaccinated people encountered the microorganism, but the person did not become ill with the infection. During such contact immune system When a person was vaccinated with the wild type of the virus, his protection was activated, and revaccination was not required. And when contact with the wild measles virus does not occur, the immune system requires an additional dose of the vaccine to maintain immunity to infection. That is why experts in the field of epidemiology and medicine have come to the conclusion that it is necessary to vaccinate adults under 35 years of age against measles.
Adults may refuse vaccinations, citing the following reason: “I’ll get sick, okay, I’m no longer a child - I’ll survive somehow.” However, remember that there are children and elderly people around you, for whom you can become a source of infection. In addition, complications of measles in adults are quite dangerous, since they can be myocarditis and conjunctivitis with damage to the cornea of the eye, hearing loss (deafness). Therefore, as a responsible and mature person, it is necessary to get vaccinated against this infection as an adult. In addition, the measles vaccine is required for all adults who come into contact with a sick person. And since almost all children today are vaccinated, the virus causes illness in adults who have not been vaccinated or have not had the infection.
Vaccination of children against measles
Children should receive the measles vaccine because the infection can cause severe neurological complications or even death. Today, the measles vaccine should be administered no earlier than 9 months of age. This is due to two circumstances - firstly, maternal antibodies protect the child up to 6 - 9 months, and secondly, at six months the baby’s immune system is not yet able to adequately respond to the introduction of the measles vaccine and form immunity - that is, the vaccination will simply be useless .The introduction of measles vaccination to infants at the age of 9 months leads to the formation of immunity in 85–90% of those vaccinated. This means that 10–15% of children do not develop immunity after vaccination at 9 months, and a second dose of the drug is necessary. When children are vaccinated at the age of 1 year, immunity is formed in 100% of children. Therefore, the World Health Organization considers the optimal time for measles vaccination to be one year old.
However, countries where the epidemiological situation regarding measles is unfavorable are forced to administer the vaccine to children as early as possible, that is, from 9 months of age. The consequence of this tactic is the presence of 10 - 15% of children who did not receive protection from infection after one dose of the drug. In this regard, in countries that introduce measles vaccination at 9 months, repeated immunization is carried out at 15–18 months so that all children can develop immunity to infection. This tactic has shown good efficiency and effectiveness.
In Russia, the epidemiological situation is not so dire, so children as young as 1 year can be vaccinated against measles. It is at this age that vaccination is scheduled in the national vaccination calendar. To prevent possible outbreaks of the epidemic in children's groups, a second dose of the vaccine is administered to activate immunity at 6 years of age, before the child enters school. This measles prevention tactic has made it possible to completely eliminate outbreaks of infection in schools, so today it is almost impossible to observe a situation where the entire class is on sick leave with the same diagnosis. And 10 years ago this situation was quite typical for Russian cities.
Measles vaccination per year
The introduction of measles vaccinations per year is determined by three main factors:1. By this age, the baby’s maternal protective antibodies, which were transmitted through the placenta, completely disappear.
2. It is the age of 1 year that is optimal for immunization against measles, since immunity is formed in almost 100% of children.
3. Children under 5 years of age are highly susceptible to measles and often become ill and experience infection with subsequent complications.
Therefore, to prevent measles infection in vulnerable children aged 1 to 5 years, it is necessary to get vaccinated as early as possible. After vaccination at 1 year of age, the child receives immunity, which reliably protects him from infection. The measles vaccine is easily tolerated by one-year-old children, rarely causing reactions that appear 5 to 15 days after the injection and pass very quickly.
In children, measles is dangerous due to its complications on the nervous system, primarily the formation of encephalitis and meningitis, as well as damage to the lungs in the form of severe pneumonia. These complications from measles occur in 1 child out of 1000 infected. And vaccination can cause complications in the form of damage to the nervous system in 1 child per 100,000 vaccinated children.
As a child gets older and gets measles, the risk of developing complications from the nervous system decreases, but the risk of other conditions, such as myocarditis, optic and auditory nerves, increases, which can result in serious deterioration in health and a significant decrease in quality of life.
How many measles vaccinations are needed?
The number of measles vaccinations depends on the age of first vaccination. So, if the first vaccine was administered to a child at 9 months of age, then there will be 4–5 vaccinations in total: the first at 9 months, then at 15–18 months, at 6 years, at 15–17 years, and at 30 years. If the first measles vaccination was given at the age of 1, then there will be 3–4 vaccinations in total, that is, the first one per year, then at 6 years, at 15–17 years, and at 30 years.If the child has not been vaccinated against measles at one year, then he is given one dose as early as possible (for example, at two, or three, or four years). After this vaccination, the next scheduled one is given at the age of six, before entering school.
If an adult or a child over 6 years of age is vaccinated for the first time, two doses of the drug are administered, with an interval of at least 1 month between them. The optimal interval in this situation between the first and second dose of the vaccine is six months.
Immunization age (vaccination calendar)
 According to the national vaccination calendar, measles vaccination is carried out at the age of:
According to the national vaccination calendar, measles vaccination is carried out at the age of:
- 1 year;
- 6 years;
- 15 – 17 years old.
- 9 months;
- 15 – 18 months;
- 6 years;
- 15 – 17 years old.
If a child over 6 years of age has not been vaccinated against measles, then two vaccines are administered with an interval of six months as soon as possible. The next vaccination schedule is at 15–17 years of age.
Where can I get a measles vaccination?
The measles vaccination can be given at the vaccination office of the clinic at your place of residence or work. In this case, you need to find out on what days measles immunization is carried out, if necessary, make an appointment and come to get vaccinated. In addition to the municipal clinic, the vaccine can be given at special vaccination centers or private clinics accredited to carry out these medical procedures. If you have other somatic diseases, the measles vaccine can be delivered in specialized immunology departments of multidisciplinary hospitals.Private vaccination centers provide the service of administering vaccinations at home, when a special team arrives, assesses the person’s condition, and decides whether the drug can be administered or not. This method of immunization allows you to minimize the risk of catching a cold or getting sick due to being in the corridors of the clinic.
Where is the vaccine injection given?
 The measles vaccine is administered subcutaneously or intramuscularly. The most preferred places for administering the drug are the outer part of the shoulder at the border of the middle and upper third, the thigh or the subscapular region. At one year of age, children are vaccinated in the hip or shoulder, and at 6 years old - under the shoulder blade or in the shoulder. The choice of injection site is determined by the development of the muscle layer and subcutaneous tissue in the child. If there is not enough muscle on the shoulder and a lot of fatty tissue, then the injection is given in the thigh.
The measles vaccine is administered subcutaneously or intramuscularly. The most preferred places for administering the drug are the outer part of the shoulder at the border of the middle and upper third, the thigh or the subscapular region. At one year of age, children are vaccinated in the hip or shoulder, and at 6 years old - under the shoulder blade or in the shoulder. The choice of injection site is determined by the development of the muscle layer and subcutaneous tissue in the child. If there is not enough muscle on the shoulder and a lot of fatty tissue, then the injection is given in the thigh. The vaccine should not be allowed to get into the skin, since in this case a compaction will form and the drug will enter the blood slowly, as a result of which the manipulation may be completely ineffective. An injection into the buttock should also be excluded, since the fat layer is highly developed here and the skin is quite thick, which creates difficulties for the correct administration of the vaccine preparation.
Effect of the vaccine
The measles vaccination provides a person with immunity for a fairly long period of time - on average 20 years. Today, research has revealed active immunity against measles in people vaccinated up to 36 years ago. Due to such a long-lasting effect of the vaccine, many people may have a question: “Why revaccination against measles for a 6-year-old child, when only 5 years have passed since the first vaccination?” This need is due to the fact that after the first measles vaccination at 1 year of age, immunity is formed in 96–98% of children, and 2–4% remain without reliable protection. Therefore, the second is aimed at ensuring that children who have not developed immunity at all, or have a weakened one, can receive reliable protection against infection before starting school.The third immunization is carried out at 15–17 years of age complex preparation against measles-rubella-mumps. At this age, it is most important to revaccinate boys and girls against mumps and rubella, which can negatively affect the ability to bear children, and the measles component is simply additional, stimulating the maintenance and preservation of existing immunity to infection.
Measles after vaccination
The measles vaccine contains live but greatly weakened viruses that are not capable of causing a full-fledged infection. However, after the injection, delayed reactions may occur that resemble symptoms of measles. These vaccine reactions develop 5–15 days after vaccination, occur easily and go away on their own, without any treatment. It is these reactions that people mistake for vaccine-induced measles.However, a different situation may arise. The vaccination may not have led to the formation of immunity, so a child or adult who comes into contact with the virus can easily become infected and get sick. If measles-like symptoms developed between 5 and 15 days after the injection, then this is a reaction to the vaccine. If symptoms of measles are observed at any other time, then this is a full-fledged infection associated with the failure of vaccine immunity.
After measles vaccination
Since the measles vaccination is a manipulation aimed at causing an active response of the immune system in order to create immunity to infection, it is not surprising that it can provoke the development of various reactions from the body. On the first day after injection of the drug, the temperature may rise slightly, compaction and slight soreness may appear at the injection site. These symptoms go away on their own and quickly.There are also a number of delayed reactions that appear 5 to 15 days after the injection. These reactions are a variant of the norm and do not indicate pathology or disease due to vaccination. Reactions are more often formed on the first dose of the drug, and the second and subsequent ones cause consequences much less frequently.
Reaction to the vaccine
Many people consider natural vaccine reactions to be consequences of vaccination. You can call these phenomena whatever you like - the main thing to remember is that this is not a pathology, but a normal reaction of the human body, determined by its individual characteristics. Let's look at the main reactions to the measles vaccine. Fever. Temperature can be observed on the first day after vaccination, and on days 5–15. The rise in temperature in some people is insignificant, while in others - on the contrary, up to a fever of 40 o C. The temperature reaction lasts from 1 to 4 days. Since temperature does not help the formation of immunity after vaccination, it must be brought down with paracetamol or ibuprofen. High fever can lead to seizures, especially in children.
Fever. Temperature can be observed on the first day after vaccination, and on days 5–15. The rise in temperature in some people is insignificant, while in others - on the contrary, up to a fever of 40 o C. The temperature reaction lasts from 1 to 4 days. Since temperature does not help the formation of immunity after vaccination, it must be brought down with paracetamol or ibuprofen. High fever can lead to seizures, especially in children.
Vaccination measles-rubella-mumps - rash. A variety of small pink papular rashes are observed in approximately 2% of vaccinated people 5–15 days after vaccination. The rash can cover the entire body, or be located only in certain places, most often behind the ears, on the neck, face, buttocks, and arms. The rash goes away on its own and does not require treatment. If a child is prone to allergic reactions, a rash may form on the first day after the injection.
, exacerbation of existing allergies);
Gentamicin, etc.);
Imported measles-rubella-mumps vaccine
 The main difference between imported vaccines and domestic ones is the presence of protein chicken eggs, since this is the substrate that is used to grow viral particles. Russian vaccines contain quail egg protein. There are complex vaccines measles-rubella-mumps imported - MMR-II (American-Dutch), Priorix (Belgian) and Ervevax (English). There is also a monovalent vaccine only against measles - Ruvax (French).
The main difference between imported vaccines and domestic ones is the presence of protein chicken eggs, since this is the substrate that is used to grow viral particles. Russian vaccines contain quail egg protein. There are complex vaccines measles-rubella-mumps imported - MMR-II (American-Dutch), Priorix (Belgian) and Ervevax (English). There is also a monovalent vaccine only against measles - Ruvax (French). The imported measles-rubella-mumps vaccine allows you to get one shot against three infections. And domestic drugs, as a rule, are administered in the form of two injections - one for measles-rubella, and the second for mumps. In this sense, an imported vaccine is more convenient, since it involves only one injection rather than two. Reactions after vaccination with domestic and imported vaccines are observed in exactly the same number of cases.









