Human anatomy - reproductive and reproductive system. The structure and functions of the male and female reproductive systems in humans.
JOB 196
Unlike other cells of the body, sex cells have half the set of chromosomes: 23 instead of 46. Sex is determined by sex chromosomes: in men - XY, in women - XX in every cell of the body, except the sex chromosomes. Based on this, answer the questions and complete the tasks (see §63).
1. Is the chromosome set of eggs (female germ cells) the same?
If so, what sex chromosome do they contain?
Yes, the egg carries the X chromosome.
2. Is the chromosome set of sperm (male reproductive cells) the same?
No.
If not, what chromosome will they differ in?
In 21 pairs, men have 2 chromosomes - X and Y. Accordingly, sperm carry one of them, X and Y.
3. Fill out the table. Determine the sex of the child with the following combinations of sex chromosomes.
4. Answer the question, fill in the blanks.
Is the number of sperm with sex chromosome X the same or different with sex chromosome Y?
Same.
Therefore, the probability of having a boy and a girl is 1:1
As a result of her previous three pregnancies, the woman gave birth to three girls. What is the probability of having a boy during the fourth pregnancy?
The same as for the first, second, fifth and any other - 50%.
JOB 197
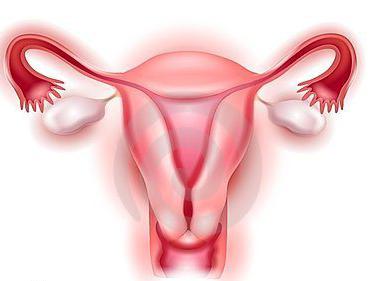
1. Name the parts of the female reproductive system corresponding to the numbers in the picture.
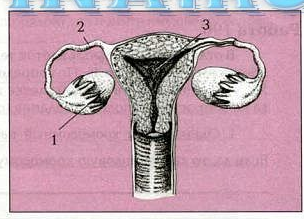
2. In which ovary (left or right) is the process of ovulation indicated?
Right.
3. How is an egg created and what happens to it in the future?
When the follicle matures, it fills with fluid and protrudes onto the surface of the ovary. The follicle bursts and the egg enters the abdominal cavity, and from there into the fallopian tube. After 12-14 days it enters the uterus.
JOB 198
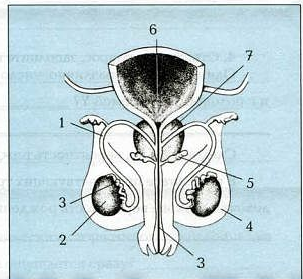
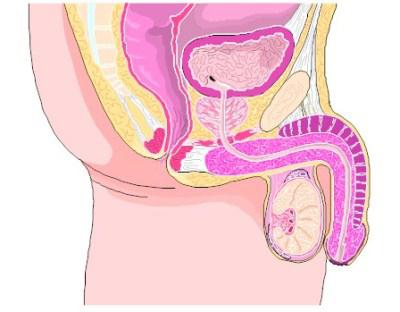
What numbers indicate the organs of the male reproductive and urinary system in the figure?
JOB 199
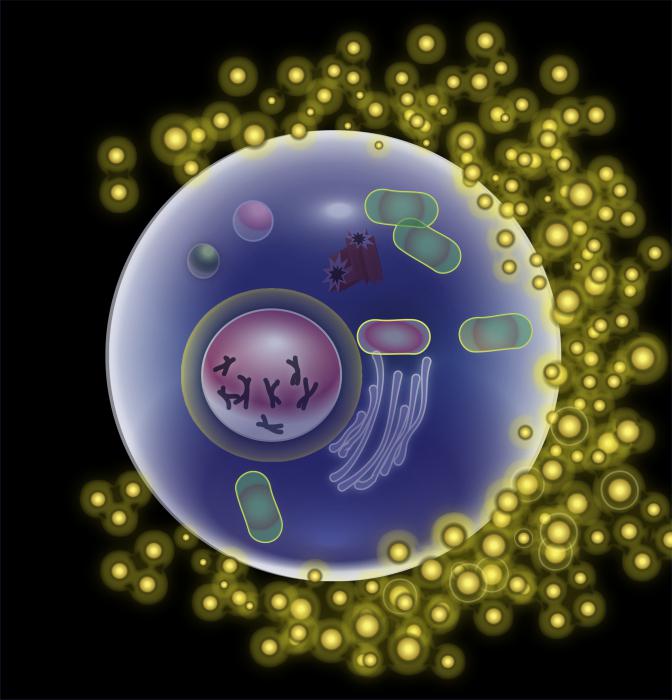
1. What process is shown in the figure?
Fertilization. 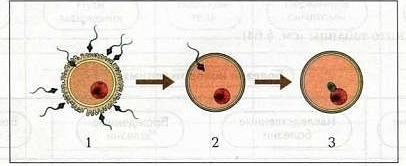
2. Where does this process take place?
In the fallopian tube.
3. How many chromosomes does a sperm have?
23 (haploid set)
4. How many chromosomes does an egg have?
23 (haploid set)
5. How many chromosomes does a fertilized egg - zygote - have?
46 (diploid set)
6. The zygote splits, and a multicellular embryo descends into the uterus. What is the significance of the villi on its surface?
With their help, the embryo adheres to the loose walls of the uterus and receives nutrients.
7. Look at the drawing. Why is the embryo retained in the uterus, but the unfertilized egg is not?
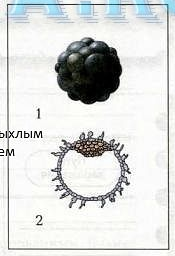
Villi contribute to this.
8. What is menstruation and how does it manifest itself?
The fertilized egg cannot attach and comes out with a loose layer separated from the uterus. This process is accompanied by bleeding.
9. What hygienic measures are necessary to prevent diseases of the male and female reproductive systems?
Maintain personal hygiene and follow-up with a doctor.
10. Why should women be examined in an examination room at least once a year?
To prevent tumors in the uterus.
Like all mammals, humans are bisexual creatures. Sexual reproduction has become established over a long period of evolution as the most common form of procreation. In this form the main role is played reproductive system. It consists of the organs responsible for the reproduction of species. In this regard, the anatomy of the human reproductive system is represented by male and female genital organs.
The main function of the former is the production and delivery of sperm (male reproductive cells) to a woman. Main function secondly, the delivery of male cells for fertilization, as well as ensuring the development of a fertilized egg. Let's look at the structure of the male and female reproductive systems in more detail:
Organs of the male reproductive system
The male penis (penis) is cylindrical in shape and consists of two cavernous bodies, as well as a spongy body. The urethra, or urethra, runs inside it. It is designed to remove urine and semen from a man’s body.
The glans is located at the outer end of the penis. It has a thickened shape, separated by a corolla and covered with very sensitive and thin skin with many nerve endings. In a calm state, the head is covered by the foreskin. When an erection occurs, the head is exposed.
At the base of the penis is a pouch of dark, wrinkled skin called the scrotum. The male sex glands (gonads) and testes (testicles), which are popularly called testicles, are located there. They produce the male hormone testosterone and also produce sperm (sperm).
Sperm produced by the testicles is located in two vas deferens, 35-40 cm long. At the moment of ejaculation (ejaculation), the seminal fluid is carried into the urethra.
The average man's semen contains approximately 300 million sperm in 3 milliliters. One sperm can move at a speed of approximately 1.5 millimeters per minute. Once in the vagina, the sperm lives for about 2 more days. However, he retains the ability to fertilize an egg only for 24 hours.
The urethra is surrounded by the prostate gland (prostate). This organ also produces seminal fluid.
At the base of the male penis are the Cooper glands. They supply clear fluid to the urethra. It is needed to neutralize the acidic environment of the urethra, which can damage sperm.
Organs of the female reproductive system
The female reproductive system, like the male one, consists of external and internal genital organs.
The external genitalia of a woman are collectively called the vulva. Directly in front of it is the pubis, which is called the “tubercle of Venus.” It is a fold of skin covered with pubic hair, which has a protective function and protects the sensitive organs located behind them.
The vulva has external borders, which are two dense folds of skin ( big lips), which are covered with pubic hair. They contain sweat glands and are permeated nerve endings. Therefore, when they are irritated, sexual arousal occurs. Between these thick folds are two thin folds that are extremely sensitive. They are called labia minora.
The labia minora grow together in their upper part, forming a kind of small cap of skin that covers a very sensitive organ of the female genital area - the clitoris. Its anatomy is such that it is extremely similar to the male penis, only in miniature. And the cap is anatomically similar to the male foreskin.
The entrance to the vagina is hidden inside the labia minora. Inside it is the hymen, which is torn during the first sexual intercourse. However, in some women the hymen may be completely absent from birth, in others it does not completely cover the entrance to the vagina, and in others it has the ability to stretch freely and does not tear. Therefore, such women can maintain their virginity, even having sexual experience.
Inner feminine reproductive system
The vagina is located inside female body and is a cylinder (tube) of muscles. It begins at the beginning of the vaginal opening and extends to the cervix. The entrance to the vagina is extremely sexually sensitive, unlike its inner walls.
The vagina is connected to the uterus through a narrow cervix. The development of the embryo occurs in this organ. The uterus communicates with the ovaries through the fallopian (uterine) tubes (oviducts). In the cavity of these organs, fertilization of the fertilized egg actually occurs. Around the entrance to the fallopian tubes, finger-like canes of skin (fringe) of the ovaries using rhythmic movements propel the fertilized egg into the uterus.
The ovaries are located on either side of the uterus, at the end of the fallopian tubes. They are designed to produce eggs and female sex hormones (estrogen and progesterone).
The egg produced by the ovary moves along the oviduct to the uterus. If a cell in the oviduct has been fertilized by a sperm, it is fixed in the uterus and is called a fertilized egg. Later it turns into an embryo.
From all that has been said, we can conclude that the organs of the human reproductive system are designed to participate in the production of gametes and hormones, ensure the process of fertilization and thereby contribute to human reproduction.
The structure and functions of the male and female reproductive systems in humans
Reproductive system- a set of organs that ensure sexual reproduction. Humans are characterized by sexual reproduction with internal fertilization. Dioecy is observed with the phenomenon sexual dimorphism(difference in characteristics of male and female individuals of dioecious species). Reproduction becomes possible with the onset of puberty. May be observed early puberty, which is associated with acceleration (acceleration of pace individual development and the growth of children and adolescents compared to previous generations). The basis of human reproduction biological(for example, sexual relations) and social(for example, love).
Structure and functions of male genital organs
|
Name |
Brief description |
functions |
|
|
Internal genital organs |
|||
|
Testicle with appendages |
Paired gonads, which are contained in the scrotum; consist of seminiferous canals and intermediate cells. The epididymis runs along the back of each testicle |
Formation of sperm and hormones (testosterone). Sperm maturation (in the epididymis for 2 weeks) |
|
|
seminal vesicles |
Paired glands between the bottom of the bladder and the rectum |
Produce a secretion that is part of sperm (provides nutrients and sperm motility) |
|
|
Prostate (prostate) |
The gland around the initial part of the urethra, located under the bladder |
Produces a secretion that is part of sperm (ensures the movement of sperm) |
|
|
Glands of the urethral bulb |
Gland near the posterior end of the penile bulb |
Produces mucus that protects the urethra from irritation from urine |
|
|
External genitalia |
|||
|
Penis (penis) |
Consists of cavernous bodies that can fill with blood (erection). Has a root, body, head with foreskin |
Provides sexual intercourse, removal of sperm, urine |
|
|
scrotum |
Protrusion of body skin |
Contains the testes, epididymis and seminal ducts |
|
Structure and functions of female genital organs
|
Name |
Brief description |
functions |
|
Internal genital organs |
||
|
ovaries |
Located in the pelvic cavity. Paired oval-shaped organs with cortical and medulla layers surrounded by a protein membrane |
Formation of gametes and hormones (estradiol and progesterone) |
|
uterine pipes |
Paired muscle formations with a funnel near the ovaries and ciliated epithelium inside |
Connect the ovaries to the uterus, transporting the egg |
|
uterus |
A hollow muscular organ made of 3 layers. Has two side and one bottom holes. Isolate the body and cervix |
Performs secretory and endocrine functions. Provides uterine development of the fetus |
|
vagina |
Tubular copulative female organ from 3 membranes: serous, muscular and mucous. Approximately 10 cm long. The mucous membrane contains glands |
Combines the uterus with the genital slit. Releases germicidal lubricant |
|
External genitalia |
||
|
shameful plot |
Formed by the pubis, labia, vestibule of the vagina, glands of the vestibule, hymen |
Provides protection, sexual feelings, secretion |
|
clitoris |
Consists of cavernous bodies and is capable of erection. Has legs, body and head |
Sexual organ |
The human reproductive system is a complex of organs through which reproduction occurs. They also determine gender characteristics and perform sexual function. Unlike other organ systems, the reproductive system begins to function only when human body ready to participate in childbirth. This occurs during puberty.
Sexual demorphism is pronounced; The human reproductive system is responsible for the formation of differences, that is, the male and female sexes differ from each other in internal and external structure.
The reproductive system, the structure of which allows men and women to produce gametes using the gonads (sex glands), is divided:
- on the external genitalia;
- internal genital organs;
Male reproductive system, histology of internal organs
The male reproductive system is represented by external (penis, scrotum) and internal (testicles and their appendages) organs.
Testicles (testes, testicles) are gonads, a paired organ within which spermatogenesis (maturation of sperm) occurs. The testicular parenchyma has a lobular structure and consists of seminiferous tubules that open into the epididymal canal. The spermatic cord approaches the other edge. During the perinatal period, the testes are in abdominal cavity, then normally descend into the scrotum.

The testes produce a secretion that is part of sperm, and also secrete androgen hormones, mainly testosterone, and in small quantities estrogen and progesterone. Together, these hormones regulate spermatogenesis and the development of the entire organism, stopping the growth of bones in length at a certain age. Thus, the formation of the entire organism is influenced by the reproductive system, the organs of which not only have a reproductive function, but also participate in humoral regulation.
In the testes there is a constant production of sperm - male gametes. These cells have a movable tail, thanks to which they are able to move against the flow of mucus in the woman’s genital tract towards the egg. Mature sperm accumulate in the epididymis, which has a system of tubules.
The accessory sex glands also play a role in the formation of sperm. The prostate gland secretes some components of sperm and substances that stimulate spermatogenesis. The muscle fibers present in the gland compress the urethra during sexual arousal, preventing urine from entering during ejaculation.
Cooper's (bulbourethral) glands are two small formations located at the root of the penis. They secrete a secretion that dilutes sperm and protects the urethra from the inside from irritating effect urine.

External male genitalia
The male reproductive system also includes the external genitalia - the penis and scrotum. The penis consists of a root, a body and a head; inside there are two cavernous and one spongy body (the urethra lies in it). In a state of sexual arousal, the corpus cavernosum fills with blood, resulting in an erection. The head is covered with thin movable skin - the foreskin (prepuce). It also contains glands that secrete a slightly acidic secretion - smegma, which protects the body from the penetration of bacteria.
The scrotum is the outer, musculocutaneous membrane of the testes. The latter performs protective and thermoregulatory functions.
Secondary male sexual characteristics
Men also have secondary sexual characteristics, which are indicators of puberty and gender differentiation. These include male-type facial and pubic hair growth, armpit hair growth, as well as growth of laryngeal cartilage, which leads to a change in voice, with the thyroid cartilage coming forward, forming the so-called Adam's apple.
Female reproductive system
The female reproductive system has a more complex structure, since it performs not only the function of producing gametes - fertilization occurs in it, and then the development of the fetus with its subsequent birth. The internal organs are represented by the ovaries, fallopian tubes, uterus and vagina. External organs are the labia majora and minora, hymen, clitoris, Bartholin's and mammary glands.
External female genitalia
The female reproductive system is externally represented by several organs:
- The labia majora are folds of skin with fatty tissue that perform a protective function. Between them there is a genital gap.
- The labia minora are two small folds of skin, resembling a mucous membrane, located under the labia majora. Inside they have muscle and connective tissue. The labia minora cover the clitoris on top and form the vestibule of the vagina below, into which the opening of the urethra and gland ducts open.
- The clitoris is a formation in the upper corner of the genital opening, measuring only a few millimeters in size. In its structure it is homologous to the male genital organ.
The entrance to the vagina is covered by the hymen. In the groove between the hymen and the labia minora there are Bartholin's glands, one on each side. They secrete a secretion that acts as a lubricant during sexual intercourse.
Together with the vagina, the external genitalia are a copulatory apparatus designed for the introduction of the penis and sperm, as well as the removal of the fetus.
Ovaries
The female reproductive system also consists of a complex internal organs located in the pelvic cavity.
The ovaries are the sex glands, or gonads, a paired oval-shaped organ located to the left and right of the uterus. During embryonic development, they form in the abdominal cavity and then descend into the pelvic cavity. At the same time, primary germ cells are laid, from which gametes will subsequently be formed. It is the endocrine glands that regulate the reproductive system, the histology of which is such that there are both organs that produce hormones and target organs that respond to humoral influences.
After maturation, the reproductive system begins to work, as a result of which ovulation occurs in the ovaries: at the beginning of the cycle, the so-called Graafian vesicle matures - a sac in which the female gamete - the egg - is formed and grows; Approximately in the middle of the cycle, the bubble bursts and the egg is released.
In addition, the ovary, being endocrine gland, produces the hormone estradiol, which is involved in the formation of the female body and many other processes, as well as in small quantities testosterone (male sex hormone). In place of the burst follicle, another gland is formed - the corpus luteum, the hormone of which (progesterone) ensures the safety of pregnancy. If fertilization does not occur, the corpus luteum dissolves, forming a scar.
Thus, the reproductive system regulates the physiological development of the body. It is the sequence of work of the follicular system and the corpus luteum system that forms the menstrual cycle, which lasts on average 28 days.
Fallopian tubes
Funnel-shaped tubes extend from the corners of the uterine fundus to the ovaries, the wide part of which faces the ovary and has a fringe-like edge. On the inside, they are covered with ciliated epithelium, that is, the cells have special cilia that make wave-like movements that promote fluid flow. With their help, the egg released from the follicle moves through the tube towards the uterus. This is where fertilization occurs.
Uterus
The uterus is a hollow muscular organ in which the embryo develops. This organ has a triangular shape; it has a bottom, a body and a neck. The muscular layer of the uterus thickens during pregnancy and is involved in childbirth, as its contraction provokes the expulsion of the fetus. The mucous inner layer grows under the influence of hormones so that the embryo can attach to it at the very beginning of its development. If fertilization does not occur, then at the end of the menstrual cycle the membrane is torn away and bleeding occurs (menstruation).
The cervical canal (cervical canal) passes into the vagina and secretes mucus, which creates a barrier that protects the uterus from environmental influences.
Vagina
The vagina is a muscular organ in the shape of a tube, covered from the inside with a mucous membrane; located between the cervix and the genital opening. The walls of the vagina are elastic and stretch easily. The mucous membrane is populated by specific microflora that synthesize lactic acid, due to which the urinary reproductive system is protected from the introduction of pathogenic microorganisms.
Secondary sexual characteristics of women
Women, just like men, have secondary gender characteristics. During puberty, they experience growth of hair on the pubis and in the armpits, and the formation of female type figure due to fat deposits in the pelvis and hips, while the pelvic bones extend in the horizontal direction. In addition, women develop mammary glands.
Mammary glands
The mammary glands are derivatives of the sweat glands, but perform the function of milk production during feeding of the baby. The rudiments of the glands are formed during the perinatal period in all people. In men, they remain in their infancy throughout their lives, since their reproductive system is not designed for lactation. In girls, the mammary glands begin to grow after the menstrual cycle is established and develop to their maximum towards the end of pregnancy.
In front of the gland there is a nipple into which the milk ducts open. Milk begins to be secreted in the alveoli under the influence of the hormone prolactin, produced by the pituitary gland as a reflex in response to irritation of nipple receptors during sucking. Lactation is also regulated by oxytocin, a hormone that contracts smooth muscle, allowing milk to move through the milk ducts.
After childbirth, colostrum is produced - a secretion yellow, containing an increased amount of immunoglobulins, vitamins and minerals. On days 3-5 of lactation, milk production begins, the composition of which changes with the age of the child. On average, lactation lasts 1-3 years. After its completion, partial involution of the glands occurs.
Thus, the female reproductive system has a complex reproductive function, ensuring gestation and birth of the fetus, as well as its subsequent feeding.
Reproductive system is a complex of organs united by a common origin, development and function that ensure the processes of sexual reproduction.
Reproductive organs:
Gonads, where germ cells are formed (testis, ovary);
Ducts through which sex cells exit the glands (duct of the epididymis, vas deferens, fallopian tube);
Organs where sex cells mature or the fetus develops (uterus, ampoules of the vas deferens);
The copulatory apparatus ensures the connection of germ cells (vagina and external genitalia).
Functions: functions of the reproductive system - production of gametes and sex hormones.
Gender: definition, classification, types of sex.
Floor- a set of characteristics by which a specific division of individuals is made, based on their morphological and physiological characteristics and allowing for the combination of the hereditary primordia of the parents in the process of sexual reproduction.
Types of floor: - chromosomal (xx, xy);
Gonadal (testicle, ovary);
Somatic;
7. - diencephalic (cerebral);
8. - hermaphroditism (false, true).
3.4 Ontogenesis and developmental anomalies of male genital organs. Ontogenesis and developmental anomalies of female genital organs.
4th week of embryogenesis – indifferent rudiment of the gonad in the form of thickening of the rudimentary epithelium of the body cavity around the mesonephric duct;
5th week of embryogenesis – formation of paramesonephric ducts;
Week 7 of embryogenesis – differentiation of the gonads by gender.
|
Source of development |
Forming organs |
|
|
in men |
in women |
|
|
Mesonephric duct |
Straight seminiferous tubules, rete testis, efferent ducts, epididymal duct, vas deferens, seminal vesicles and ejaculatory duct |
Epididymis, periovarian. (Basically the mesonephric duct is reduced). |
|
Paramesonephric duct |
Appendage of testicle, prostatic uterus. (Basically, the paramesonephric duct is reduced). |
From the unfused upper parts are the fallopian tubes. The fused lower parts include the uterus and vagina. |
Anomalies in the development of organs of the male reproductive system:
Anomalies of testicular development: testicular hypo- and aplasia, testicular retention (cryptorchidism), testicular ectopia, testicular inversion, polyorchidism, synorchidism.
Anomalies of the penis: micropenia, macropenia, duplication (diphallia), phimosis.
Urethral anomalies: epispadias, hypospadias, duplication of the urethra, congenital strictures, urethral diverticula.
Anomalies in the development of organs of the female reproductive system:
Ectopic ovary, accessory ovary, ovarian hypoplasia
Duplication of organs: uterus and vagina; bicornuate uterus; separated uterus and vagina
Vaginal atresia and hypoplasia.
5. Testicle: sources of development, structure, its intrasecretory part. The process of descent of the testicle and the formation of its membranes. Age characteristics.
Testicular development:
2nd month – cords of the testis (coelomic epithelium of the visceral layer of the splanchnotome), developing around the mesonephric ducts;
3 month – the tunica albuginea, interstitial tissue, is formed from the mesenchyme surrounding the future gland;
4th month – formation of the testicle and vas deferens from the mesonephric duct, connection of the excretory ducts of the testicle and epididymis;
The process of descent of the testicles: 3 month - in the iliac region; 6 month – at the internal inguinal ring; 7-8 months - passes through the inguinal canal.
Age Features: Testicles
Structure
Transverse section of the left part of the scrotum and left testicle. (en)
vas deferens
tunica vaginalis
head of epididymis
epididymal body
upper end of testicle
lateral surface of the testicle
tail appendage
anterior margin of testis
lower end of testicle
Dimensions and position
The testicles are located in the scrotum and descend there from the abdominal cavity, usually at birth (the absence of a testicle in the scrotum occurs in 2-4% of full-term, 15-30% of premature newborns and 1% of 1-year-old boys - see cryptorchidism). This is necessary for normal sperm maturation, which requires a temperature regime a few tenths of a degree lower than the temperature in the abdominal cavity.
Usually the testicles are located on at different levels and may differ in size - often the left one is lower and larger than the right one. The shape of the testicle resembles a slightly flattened ellipsoidal body, 3.5-5 cm long, 2.3-3.5 cm wide, weighing 15-25 g. In an adult healthy Caucasian male, the average testicular volume is about 18 cm³, ranging from 12 cm³ up to 30 cm³.
Prostate gland, seminal vesicles: sources of development, topography, structure, functions. Age characteristics.
Prostate gland (synonym: prostate) - exocrine tubular-alveolar gland male body mammals. The prostate gland varies significantly among different types in anatomical, physiological and chemical terms.
Human prostate gland
In humans, the prostate gland is an unpaired androgen-dependent organ located below the bladder. It covers the initial part of the urethra on all sides. The excretory ducts of the prostate gland open into the urethra.
The secretion produced by the prostate, released during ejaculation, contains immunoglobulins, enzymes, vitamins, citric acid, zinc ions, etc. This secretion is also involved in the liquefaction of the ejaculate.
The functions of the prostate are controlled by pituitary hormones, androgens, estrogens, and steroid hormones.
Functions of the prostate gland
Production of prostatic juice, which is the basis for sperm.
Production of biologically active substances (prostaglandins).
Plays the role of a valve - it closes the exit from the bladder during an erection.
Creates a feeling of orgasm due to the developed innervation system.
The amount of secretion increases sharply under the influence of parasympathetic impulses and androgens.
Topography
The prostate consists of 30-50 glands, forming the substantia glandularis, and muscle substance, substantia muscularis, representing the stroma of the gland. The glands open into the prostatic part of the urethra through the ductuli prostatici. Since the glandular part occupies only about 2/3 of the tissues enclosed in the capsule, according to the new terminology the term “prostate gland” is not used.
The prostate is located in the middle, subperitoneal floor of the small pelvis. It has a cone-shaped shape and is directed with its apex downwards, towards the urogenital diaphragm. The base of the prostate is located higher up, just below the bottom of the bladder. The prostate has two lobes and an isthmus. In lobes it covers the initial part of the urethra emerging from the bladder. The prostate has a well-defined visceral fascial capsule, capsula prostatica (Pirogov-Retsia), on all sides except the base, from which mm extend to the pubic bones. (ligg.) puboprostatica.
Age features:
Prostate
The structure of the external male genitalia. Age characteristics.
The male genital organs are divided into external and internal. Many authors classify only the penis and scrotum as external genital organs, and testicles, epididymis, vas deferens, paraurethral and bulbourethral glands, prostate gland and seminal vesicles as internal genital organs. From our point of view, the most reasonable thing in this case would be to divide the location of the genital organs relative to the pelvic cavity. The external ones will include the penis, scrotum, testicles and their appendages, and the internal ones will include the prostate gland and seminal vesicles. The vas deferens and urethra with the paraurethral and bulbourethral glands then occupy an intermediate position, located partly inside and partly outside the pelvic cavity. The penis consists of a head, a shaft and a root, which is attached by ligaments in front and below the pubis to the symphysis area. The shaft and root of the penis are formed from the two cavernous bodies. The corpus spongiosum surrounds the urethra, which passes through the penis, and forms the glans in the distal part. The edge of the head fuses with the cavernous bodies, forming a thickening - the corolla, behind which the coronary groove is located. The shaft of the penis is covered with thin, easily removable skin, which in the area of the coronary sulcus forms a fold (foreskin), covering the glans and forming the preputial sac. On the inner sheet foreskin there are a large number of sebaceous glands. In the lower part, the foreskin is attached to the scrotum by a frenulum. The size of the penis is very variable and ranges from 5-7 cm to 10-15 cm or more. The penis is saturated with a large number of nerve endings. Blood supply is carried out through two parallel arteries of the penis (a. penis), which are divided into bulbous, urethral, deep and superficial arteries. Venous outflow occurs through the superficial and deep veins of the penis. Innervation involves the inferior hypogastric plexus, thoracolumbar and sacral sections spinal cord, as well as the higher nerve centers of the spinal cord cortex.
Age features:Testicles: before puberty, the system of testicular tubules is not developed, the membranes are poorly expressed; intensive growth - during puberty.
Epididymis: grows slowly in the first 10 years; In newborns, the appendage of the testicle and the appendage of the epididymis are well expressed.
Vas deferens: thin, ampulla poorly defined.
Prostate: located high, round in shape, glandular tissue actively develops during puberty.
Seminal vesicles: in newborns they are located relatively high, the surface is smooth.
Penis: the foreskin covers the head, the cavernous bodies are poorly developed, the spongy body is well developed, but the bulb is small.
Scrotum: newborns are relatively large in size, the skin is non-pigmented, and the sebaceous glands are poorly developed.
Ovary: sources of development, structure, its intrasecretory part. Age characteristics.
Age features:Ovaries: in newborns, they are cylindrical in shape, located high outside the pelvic cavity, have a smooth surface, and primary primordial follicles are in the cortex. During the period of second childhood (8-12 years), the shape becomes ovoid. In adolescence, irregularities and bumps appear on their surface, caused by swelling of the maturing follicles. The ovaries (ovaria) are a paired female reproductive gland located in the pelvic cavity. An egg matures in the ovary, which is released into the abdominal cavity at the time of ovulation, and hormones are synthesized that enter directly into the blood.
The ovary of an adult woman has an oval shape, length 2.5-3.5 cm, width 1.5-2.5 cm, thickness 1-1.5 cm, weight 5-8 g. The right ovary is always larger than the left. The medial surface of the bladder faces the pelvic cavity, the lateral surface is connected by the ligament that suspends the bladder to the side wall of the pelvis. The posterior edge of the uterus is free, the anterior edge is mesenteric and is fixed by a fold of the peritoneum (the mesentery of the uterus) to the posterior layer of the broad ligament of the uterus. Most of the jaundice is not covered by peritoneum. In the area of the mesenteric edge of the bladder there is a depression through which vessels and nerves pass - the gate of the bladder. One end of the bladder (tubal) approaches the funnel of the fallopian tube, the other (uterine) is connected to the uterus by its own ligament of the bladder. Next to the bladder between the leaves of the broad The ligaments of the uterus contain rudimentary formations - the epididymis (epophoron) and the periovary (paroophoron).
Uterus: sources of development, topography and structure. Age characteristics.
The uterus (Latin uterus, Greek ὑστέρα) is an unpaired hollow muscular organ in which the embryo develops and the fetus is born. The uterus is located in the middle part of the pelvic cavity, between the bladder in front and the rectum in the back, mesoperitoneally. From below, the body of the uterus passes into a rounded part - the cervix. The length of the uterus in a woman of reproductive age is on average 7-8 cm, width - 4 cm, thickness - 2-3 cm. The weight of the uterus in nulliparous women ranges from 40 to 50 g, and in those who have given birth reaches 80 g. Such changes arise from - for muscle hypertrophy during pregnancy. The volume of the uterine cavity is ≈ 5 - 6 cm³.
The uterus has significant mobility and is located in such a way that its longitudinal axis is approximately parallel to the axis of the pelvis. When empty bladder the fundus of the uterus is directed forward, and its anterior surface is directed forward and downward; This forward tilt of the uterus is called anteversio. In this case, the body of the uterus, bending forward, forms an angle with the cervix, open anteriorly, anteflexio. When the bladder is stretched, the uterus can be tilted back (retroversio), its longitudinal axis will go from top to bottom and forward. Backward bending of the uterus (retroflexio) is a pathological phenomenon.
The peritoneum covers the front of the uterus to the junction of the body with the cervix, where the serous membrane folds over the bladder. The depression of the peritoneum between the bladder and the uterus is called excavatio vesicouterine. The anterior surface of the cervix is connected through loose tissue to the posterior surface of the bladder. WITH back surface The peritoneum of the uterus continues for a short distance onto the posterior wall of the vagina, from where it bends onto the rectum. The deep peritoneal pocket between the rectum at the back and the uterus and vagina at the front is called excavatio rectouterine. The entrance to this pocket is limited from the sides by folds of the peritoneum, plicae rectouterinae, which extend from the posterior surface of the cervix to the lateral surface of the rectum. In the thickness of these folds, in addition to connective tissue, there are bundles of smooth muscle fibers, mm. rectouterini.
Structure: The uterus is divided into the cervix, body and fundus.
Age features:Uterus: in newborns, it is cylindrical in shape, inclined anteriorly, located high, the wall is thin; neck – thick, dense; the cervical canal is wide, usually contains a mucus plug; the vaginal part of the cervix is poorly developed. The uterine ligaments are weak.
During the second childhood, the uterus becomes rounded and its fundus expands. During adolescence it becomes pear-shaped.
Fallopian tube: sources of development, topography and structure. Age characteristics.
The fallopian tubes (oviducts, fallopian tubes) are a paired tubular organ. In fact, the fallopian tubes are two thread-like canals of standard length 10 - 12 cm and a diameter not exceeding a few millimeters (from 2 to 4 mm). The fallopian tubes are located on both sides of the fundus of the uterus: one side of the fallopian tube is connected to the uterus, and the other is adjacent to the ovary. Through the fallopian tubes, the uterus is “connected” to the abdominal cavity - the fallopian tubes open with a narrow end into the uterine cavity, and with an expanded end - directly into the peritoneal cavity. Thus, in women, the abdominal cavity is not sealed, and any infection that has the opportunity to enter the uterus causes inflammatory diseases not only of the reproductive system, but also of the internal organs (liver, kidneys), and peritonitis (inflammation of the peritoneum). That is why obstetricians and gynecologists at our Euromedprestige medical center strongly recommend coming for an examination to a gynecologist once every six months. Such a simple procedure as an examination prevents complications of inflammatory diseases - the development of precancerous conditions - erosion, ectopia, leukoplakia, endometriosis, polyps. The fallopian tube consists of:
Isthmus
Uterine part.
The walls of the fallopian tube, much like the uterus and vagina, in turn consist of a mucous membrane covered with ciliated epithelium, a muscular layer and a serous layer.
The infundibulum is the widened end of the fallopian tube that opens into the peritoneum. The funnel ends in long and narrow outgrowths - fimbriae, which “encompass” the ovary. The fimbriae play a very important role - they vibrate, creating a current that “sucks” the egg released from the ovary into the funnel - like into a vacuum cleaner. If something in this infundibulum-fimbria-ovum system fails, fertilization can occur directly in the abdominal cavity, resulting in an ectopic pregnancy.
Following the funnel is the so-called ampulla of the fallopian tube, then the narrowest part of the fallopian tube - the isthmus. Already the isthmus of the oviduct passes into its uterine part, which opens into the uterine cavity through the uterine opening of the tube. Thus, the main task of the fallopian tubes is to connect the upper part of the uterus to the ovary. The fallopian tubes have dense, elastic walls. In a woman’s body, they perform one, but very important function: in them, as a result of ovulation, fertilization of the egg with sperm occurs. Along these lines, the fertilized egg passes into the uterus, where it strengthens and develops further. The Fallopian tubes serve specifically for fertilization, carrying and strengthening the egg from the ovary into the uterine cavity.
Age features: Fallopian tubes: convoluted, very narrow, fimbria and muscle layer are poorly developed, folds of the mucous membrane are well defined
Vagina: sources of development, topography and structure. Age characteristics.
The vagina is an easily stretchable elastic muscular tube with a depth of 7-12 centimeters and a diameter of 2-3 centimeters, which starts from the cervix and passes into the genital slit. The vagina is a genital organ involved in the process of sexual intercourse, as well as childbirth.
The walls of the vagina, depending on their location, are divided into anterior and posterior, starting at the cervix, they form the vaginal vault, and in the lower part they pass into the vestibule. In the absence of any abnormalities, the vaginal walls are pale pink and soft to the touch, but when pregnancy occurs, they change color and become darker.
In a woman without pathologies who has reached puberty, the vaginal microflora should be dominated by acidophilic lactobacilli, which include bifidumbacteria (they should be about 10% of the microflora), peptostreptococci (about 5%) and peroxide (they should be the majority). Lactobacilli produce lactic acid and also stimulate local immunity and produce some enzymes (for example, hydrogen peroxide) to fight pathogenic microorganisms.
If a woman is healthy, there must be an acidic environment in the vagina, which normally ranges from 3.5 to 4.5 pH. The acidic environment destroys the majority of sperm that enter the vagina, that is, a kind of “natural selection” occurs, as a result of which only the strongest sperm that penetrates the vagina is able to fertilize the egg. The presence of an acidic environment also ensures the destruction harmful microbes that enter the vagina in one way or another, or, if microorganisms do get in, prevents their reproduction, thus, the acidic environment ensures the health and cleanliness of the vagina for its normal functioning.
Normally, without the presence of infections, the amount of discharge and its nature depend on the menstrual cycle and are subject to the influence of hormones. Before menstruation, the discharge is creamy, whitish in color, with a sour odor; in the middle of the menstrual cycle, the discharge is similar to egg white, viscous, there is a lot of it; after menstruation, the discharge is transparent and few in number.
In addition to the vaginal glands, the glands of the vestibule and the cervical canal also take part in the formation of discharge from the genital tract. The amount depends on the predominance of certain microbes in the microflora; in women of reproductive age, lactobacilli should normally predominate. If pathogenic microorganisms begin to predominate, unpleasant symptoms may appear - increased discharge, itching, burning, in which case it is necessary to see a gynecologist to determine the causes of the pathology.
Age features:Vagina: newborn girls are short, arched, high arches, folds of the mucous membrane are pronounced, the muscular layer is poorly developed; The vestibule of the vagina is deep, limited in the posterior third by the labia majora, and in the anterior third by the labia minora. The hymen is dense.
The structure of the external female genitalia. Age characteristics.
The structure of the external genitalia (vulva)
The structure of the female external genitalia includes:
labia majora
labia minora
vestibule of the vagina
large glands of the vestibule - the so-called Bartholin glands.
Age features:Labia majora: in newborn girls they are small, loose, as if swollen. Labia minora: not completely covered by large ones.
Perineum: definition, classification. Features of the structure of the male and female perineum.
The perineum is the area between the pubic symphysis in front, the apex of the coccyx in the back, the ischial tuberosities and the sacrotuberous ligaments on the sides. It is the lower wall of the body, closing the small pelvis from below, through which the urethra, rectum, and also the vagina (in women) pass. The perineum has the shape of a diamond and is divided by a conventional line connecting the ischial tuberosities into two unequal triangular areas: the anterior - genitourinary area , where the urogenital diaphragm is located, and the posterior - anal region formed by the pelvic diaphragm.
The muscles of the urogenital diaphragm are divided into superficial and deep. The superficial muscles include the superficial transverse perineal muscle, the ischiocavernosus muscle, and the bulbospongiosus muscle (Fig. 1). The superficial transverse muscle of the perineum strengthens the tendon center of the penis. The ischiocavernosus muscle in men surrounds the peduncle of the penis, some of the fibers are directed to the rear of the penis and pass through tendon stretching into the tunica albuginea. In women, this muscle is poorly developed, goes to the clitoris, and participates in its erection. The bulbospongiosus muscle in men begins on the lateral surface of the corpus cavernosum and, meeting the muscle of the same name on the opposite side, forms a suture along the midline of the corpus spongiosum. The muscle promotes the ejaculation of sperm and urination. In women, the muscle covers the opening of the vagina (Fig. 2) and, when contracted, narrows it. The deep muscles of the urogenital diaphragm include the deep transverse perineal muscle and the external urethral sphincter. The deep transverse perineal muscle strengthens the urogenital diaphragm. In its thickness, the bulbourethral glands lie in men, and the large glands of the vestibule in women. The external urethral sphincter surrounds the urethra; in women, this muscle also surrounds the vagina. The pelvic diaphragm is formed by the levator ani muscle, the coccygeus muscle and the external sphincter anus. The levator ani muscle covers the rectum on both sides; in women, some of the fibers are woven into the vaginal wall, and in men, into the prostate gland. Muscle strengthens and lifts pelvic floor, raises the final section of the rectum, in women it narrows the entrance to the vagina. The coccygeus muscle complements and strengthens the muscular arch of the pelvic diaphragm from behind. The external anal sphincter surrounds the anus, closing it when it contracts. The fascia covering the muscles of the genitourinary diaphragm, at the posterior edge of the superficial transverse perineal muscle, is divided into three (Fig. 3): the upper one, covering the inner (upper) surface of the muscles of the genital diaphragm; lower, passing between the deep and superficial muscles of the perineum; superficial, covering the superficial muscles of the penis from below and in men passing into the fascia of the penis. The inferior and superior fascia at the anterior edge of the smooth transverse perineal muscle form the transverse perineal ligament. In the P. area, on both sides of the anus, there is a paired depression - the ischiorectal fossa. It has a prismatic shape and is filled with fatty tissue, contains internal genital vessels and the pudendal nerve. Its apex corresponds to the lower edge of the tendinous arch of the fascia of the pelvis. The lateral wall is formed by the lower 2/3 of the obturator internus muscle and the inner surface of the ischial tuberosity. The medial wall is formed by the inferior surface of the levator ani muscle and the external anal sphincter; posterior wall - posterior bundles of the levator ani muscle and the coccygeus muscle; anterior - transverse muscles of the perineum. The fiber filling the ischiorectal fossa continues into the pararectal tissue.









